The cervix is the lower part of the uterus (womb) that extends into the upper end of the vagina.
Cervical cancer develops in the cervix, the narrow outer end of the uterus that extends into the vagina. When diagnosed early, cervical cancer is curable and patients have an excellent chance of recovery.Most cervical cancers begin in an area called the transformation zone, where the inner part of the cervix closest to the uterus (the endocervix) meets the outer part of the cervix closest to the vagina (the ectocervix).
Every year, approximately 11,000 women are diagnosed with cervical cancer and about half of those women are between the ages of 35 and 55. The majority of cases are caused by exposure to the human papillomavirus (HPV), a common sexually transmitted disease. HPV affects up to 80 percent of females and males in their lifetime. Many cases of HPV clear on their own, but certain types of HPV can cause cervical, vulvar and vaginal cancer in females.
In its early stages, cervical cancer usually has no symptoms. It develops slowly, beginning as a pre-cancerous condition called dysplasia. Symptoms of cervical cancer often do not begin until the cancer spreads into nearby tissue.
As cervical cancer grows, symptoms may include:
- Continuous vaginal discharge, which may be pale, watery, pink, brown, bloody or foul-smelling
- Abnormal vaginal bleeding between periods, after intercourse, or after menopause
- Periods become heavier and last longer than usual
- Any bleeding after menopause
- Pain during intercourse
These symptoms can also be caused by other conditions, so it is best to visit KIMS HOSPITALS for a diagnosis.
Causes and Risks of cervical cancer
Anything that increases a woman’s chances of getting HPV or decreases her ability to get Pap smears is a risk factor for cervical cancer.
HPV is spread by sexual contact and is the cause of almost all cases of cervical cancer, as well as many vaginal and vulvar cancers. HPV may cause the cells in the cervix to change. If abnormal cells are not found and treated, they may become cancer.
As many as 80% of men and women who have had sex have HPV. Usually the body’s immune system eliminates the virus, and most people never know they have it. While most women with HPV will not get cervical cancer, they should be aware of the risk and have regular Pap tests.
Smoking and a weakened immune system (caused by a condition such as HIV/AIDS) can also greatly increase the risk of developing cervical cancer.
Cervical cancer risk factors include:
- Age: The risk of cervical cancer increases with age. It is found most often in women over the age of 40. However, younger women often have precancerous lesions that require treatment to prevent cancer.
- Smoking: Cigarette smoke contains chemicals that damage the body’s cells. It increases the risk of precancerous changes in the cervix, especially in women with HPV.
- Sexual behavior: Certain types of sexual activity may increase the risk of getting HPV infection. These include: 1) Multiple sexual partners, 2) high-risk male partners, 3) first intercourse at an early age and 4) not using condoms during sex.
Other cervical cancer risk factors include:
- Lack of regular Pap tests
- Having a sexually transmitted disease (STD), including chlamydia
- Diethylstilbestrol (DES) exposure before birth: This drug was used between 1940 and 1971 to help women not have miscarriages. Women whose mothers took DES during pregnancy have a high risk of vaginal and cervical cancers.
- HIV infection
- Weakened immune system: Having an organ transplant or taking steroids raises the risk of developing cervical cancer.
- Being overweight or not eating a healthy diet
Not everyone with risk factors gets cervical cancer. However, if a woman does have risk factors it’s a good idea to discuss them with a health care provider.
Cervical cancer is classified based on the type of cell where it develops. The most common types of cervical cancer are:
Squamous cell carcinoma (cancer): This is the most common type of cervical cancer and is found in 80% to 90% of cases. It develops in the lining of the cervix.
Adenocarcinoma: This type of cervical cancer develops in gland cells that produce cervical mucus. About 10% to 20% of cervical cancers are adenocarcinomas.
Mixed carcinoma (cancer): Occasionally, cervical cancer has features of squamous cell carcinoma and adenocarcinoma.
In rare instances, other types of cancer, such as neuroendocrine (small and large cell cervical cancer), melanoma, sarcoma and lymphoma, are found in the cervix.
At one time, cervical cancer was considered one of the most serious cancers for women. But thanks to effective screening with the vaginal Pap smear (also called a Pap test), which can detect cervical precancers and cancers early on
More than 90 percent of cervical cancers today are caused by infection with the human papillomavirus (HPV), a virus so common that more than two-thirds of sexually active women are infected with it at some point.
In part because cervical cancer tends to grow so slowly, there are a number of measures that a woman can take to prevent it from spreading and becoming advanced:
- Have regular Pap smears to screen for any changes in the cells of the cervix.
- Use condoms regularly to protect yourself from getting HPV.
- Discuss HPV vaccination with your doctor.
Preventing HPV with Condoms
Other than the presence of genital warts, there is no way of knowing whether a sexual partner is infected with HPV. While condoms do not provide complete protection — HPV can spread through physical contact with infected areas of the mouth, genitalia, and anus — the American Cancer Society reports that using condoms can reduce the rate of HPV infection by about 70 percent. Using condoms regularly also protects against various other sexually transmitted diseases.
HPV Vaccination
Gynecologic Surgeon Carol Brown Discusses Importance of HPV Vaccine
Watch Mem The first vaccine approved by the US Food and Drug Administration was Gardasil®. The vaccine specifically targets HPV types 16 and 18, which cause about 70 percent of cervical cancer cases, and types 6 and 11, which cause approximately 90 percent of cases of genital warts. The vaccine can only be used to prevent an HPV infection; it is not meant for women who already are infected.
Additional studies are under way to identify vaccines that target other types of HPV linked to cervical cancer, help the immune systems of men and women already infected with HPV to destroy the virus, and aid women with advanced or recurrent cervical cancer.
Cervical Cancer Screening
Your doctor can use a Pap smear or liquid-based cytology test to screen for cervical dysplasia (precancer) and cervical cancer.
Pap smear
A typical Pap smear involves four steps:
- The doctor inserts a lubricated instrument into your vagina to enlarge the opening.
- He or she takes a sample of mucus and cells by gently scraping your cervix.
- The doctor sends the tissue samples to a lab for analysis.
- If any irregularities are found, your doctor will suggest next steps.
A Pap smear test isn’t usually painful, although some women experience minor discomfort.
Getting regular Pap smears helps your doctor detect any changes in the cells of your cervix, including the presence of the HPV virus. Early detection can affect your treatment options if cancerous changes are detected in the cervix. we strongly recommend that even women who have been vaccinated against HPV get regular Pap smears.
Liquid-Based Cytology
Liquid-based cytology (for example, ThinPrep®) can detect changes in the cervix as well as testing for HPV. If your Pap smear reveals that you have something called atypical squamous cells of undetermined significance (ASCUS), liquid-based cytology can give a more complete picture of what’s going on.
The first part of liquid-based cytology is similar to a Pap smear. Your doctor inserts a lubricated instrument into the vagina and gently removes a tissue sample. The key difference from a Pap smear is that the tissue sample that gets sent to the lab is of a higher quality because it has been placed in a special liquid, processed in a machine, and then placed on a slide for examination.
These types of tests are an effective way to detect any changes and understand what’s happening in your cervix so that we can take quick action to stop any more growth or changes in the tissue. They’re also vital for diagnosing and customizing a treatment plan for you.
Detecting changes in cells in the cervix as early as possible can prevent cancer or make it easier to treat. Tests including a Pap test and a human papillomavirus (HPV) test are used to look for these changes. (A Pap test is also called a Pap smear, cervical cytology testing, or liquid-based cytology.)
| Age Group | Recommendation |
| Women younger than 21 | No routine Pap test screening |
| Women age 21 to 29 | Pap tests every three years |
| Women age 30 to 65 | Pap test alone every three years or an HPV test along with a Pap test every five years |
| Women over 65 | No screening necessary if previous screening guidelines have been followed and the woman is not at a high risk for cervical cancer |
SPECIAL CONSIDERATIONS FOR MORE FREQUENT SCREENING
Some women should be screened more often. These include women who have a weakened or compromised immune system, who have had precancerous lesions, or whose mothers used the drug diethylstilbestrol while they were pregnant. Talk with your doctor to learn if these circumstances may apply to you.
Many women come us after they have had an abnormal Pap smear that indicates cancerous changes in the cervix during a routine visit to the doctor. When you come to us, our doctors will likely examine the cervix, take a biopsy of cervical tissue, and perform other tests to assess the stage of the cancer.
We may perform one or more of the following tests and procedures:
PAP SMEAR
A Pap smear is a test most commonly used to screen for and detect the possibility of cervical cancer or precancer, called dysplasia.
To perform a Pap smear, the doctor inserts a lubricated instrument called a speculum into the vagina to enlarge the opening, and takes a sample of mucus and cells by gently scraping the cervix. Though the procedure is generally not painful, some women experience a few seconds of minor discomfort.
The tissue samples are then sent to a lab at to be analyzed under a microscope by one of our expert pathologists. Collection, sampling, screening, and interpretation of Pap smears require considerable experience and skill to ensure an accurate diagnosis.
LIQUID-BASED CYTOLOGY
With a Pap smear, cells are applied to a slide and then stained and examined in the laboratory. With liquid-based cytology, the cells are obtained in the same manner as they are for a Pap smear, but instead of being stained they are placed in a liquid, processed in a machine, and then placed on a slide. This test provides higher-quality samples than a Pap smear.
COLPOSCOPY AND BIOPSY
If a Pap smear or liquid-based cytology test shows an abnormality, your doctor may perform a colposcopy, in which a lighted magnifying instrument attached to magnifying binoculars (a colposcope) is used to examine your cervix.
Your doctor may also perform a biopsy at the same time, removing a tiny section of the surface of the cervix to examine under the microscope. One of our specially trained pathologists will examine the sample to see whether it contains abnormal or cancerous cells.
CONE BIOPSY (CONIZATION)
If abnormal cells are found or if a diagnosis is not clear after a colposcopy, it may be necessary to have minor surgery to remove a slightly larger piece of tissue from the cervix. This procedure is called a cone biopsy, or conization. In addition to helping to confirm a diagnosis, a cone biopsy can serve as an initial treatment, to simultaneously remove any precancerous or cancerous cells.
IMAGING TESTS
Our doctors may order a chest x-ray, CT scan of the abdomen and pelvis, and/or an MRI scan if there is reason to believe that the cancer has spread, or metastasized, beyond the cervix to other parts of the body.
Staging
Regardless of whether you are treated at our hospital or at another institution, the stage of the cancer will largely determine the treatment approach that your doctor recommends.
Cervical cancer is classified into several stages:
CARCINOMA IN SITU/PRECANCERS (STAGE 0) —
The first stage of cervical cancer is carcinoma in situ (also known as precancer or severe dysplasia), in which a group of abnormal cells has started to grow but has not yet spread to nearby tissues. Because stage 0 “precancers” are likely to eventually spread deeper into the tissue and become cancerous, they should be treated.
EARLY CERVICAL CANCER (STAGES I–IIA) —
Although more extensive than stage 0, these cancers are still limited to the cervix.
ADVANCED CERVICAL CANCER (STAGES IIB–IVA) —
Cervical cancer that has spread beyond the cervix and invaded the surrounding pelvic tissues in the vagina, rectum, or bladder is known as locally advanced cervical cancer.
STAGE IVB AND RECURRENT CERVICAL CANCER —
Cervical cancer that has spread beyond the pelvis (into the lungs or liver, for example), or has returned following initial therapy, is placed in this category.
The outlook for women with cervical cancer has never been better. And our doctors and specialists are always looking for new ways to improve the treatment options for women with this disease.
Each year, approximately 200 women with cervical cancer, and 50 with invasive disease, come to us for care. And we strive to provide all of them with the best outcomes possible. For example, women with advanced and recurrent disease who come to us for surgery benefit from outcomes that are among the best in the world.
Early-stage cervical cancer can often be treated with surgery. It’s possible you may not even need other forms of treatment, such as chemotherapy or radiation. The key to treating early-stage cancers or precancers is to catch them early.
Treatment for advanced cervical cancer
Our doctors use an approach called sentinel lymph node mapping to measure your cancer’s potential to metastasize (spread) to other parts of the body. This information can help your treatment team determine the right plan of care for you.
For advanced cervical cancers that may spread or have begun to metastasize, your treatment team may use a combination of surgery, radiation therapy, or chemotherapy in your plan of care. Our researchers are also working on better chemotherapy drugs for advanced cervical cancers through our program of clinical trials.
Our multidisciplinary team will devise a treatment strategy for you based on the stage of the cervical cancer, the size of the tumor, the surrounding tissues that may be affected, and whether the cancer has spread to other parts of the body. We also take into consideration your age and whether you wish to have children.
The earlier that cervical cancer is diagnosed and treated, the more likely it can be effectively cured. We typically treat cervical cancer with surgery, in some cases combined with radiation therapy, chemotherapy, or both.
For early-stage cancers in which abnormal cells are found in the cervix, our doctors may recommend a loop electrosurgical excision procedure (LEEP), in which an electrical current through a thin wire loop is used to remove the sample tissue. LEEP takes only about ten minutes under local anesthetic.
Alternatively or in addition to a LEEP procedure, our doctors may recommend a cone biopsy (conization) to more precisely remove a cone-shaped piece of tissue from the cervix with a scalpel. A cone biopsy is performed in an operating room and may include general anesthesia.
More than 90 percent of early-stage cancers are treated successfully with these surgical procedures and do not require any further treatment.
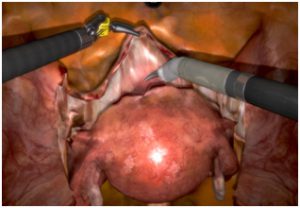
MINIMALLY INVASIVE SURGERY
For early-stage cervical cancers that are confined to the cervix, our doctors may recommend a hysterectomy, a type of surgery that involves removing the uterus entirely. The surgeon may also need to remove some tissue next to the uterus and cervix, as well as lymph nodes from the pelvis, to examine them for cancer cells.
At , the majority of these operations, known as radical hysterectomies, are performed minimally invasively — either with laparoscopy or robotics. Our surgeons have been leaders in adopting these techniques, which typically offer several advantages over traditional, open abdominal surgery for early-stage as well as more-advanced cervical cancer, such as shorter hospital stays, less risk for infection, and lower cost.
With laparoscopy, a thin, lighted tube with a video camera at its tip (a laparoscope) is inserted through a tiny incision in the abdominal wall. The surgeon can operate through this minor surgical “port” using specially designed surgical instruments.
We were also the first cancer hospital to acquire the state-of-the-art robotic da Vinci® Surgical System platform to assist in minimally invasive cancer surgeries. The use of this system during surgery can often result in less pain and faster recovery for patients.

To remove as few pelvic lymph nodes as possible when assessing the extent to which cervical cancer has spread, our doctors pioneered an approach called sentinel lymph node mapping (or intraoperative lymphatic mapping). Today, we are one of the few cancer hospitals in the United States using this approach.
During many cervical cancer surgeries, we use a dye that can be traced with imaging techniques to identify the first lymph node (the sentinel node) to which cancer cells would travel after leaving the cervix. If this node is free of cancer cells, our surgeons do not remove additional lymph nodes. If the sentinel node does contain cancer cells, the surgeon removes additional lymph nodes for further examination.
The goal of using this technique is to treat the cancer while removing as few lymph nodes as possible, which can result in a shorter surgery and fewer side effects such as swelling of the legs, known as lymphedema.
FERTILITY-SPARING RADICAL TRACHELECTOMY
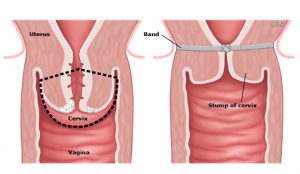
Radical Trachelectomy–During the operation, the outlined area — which includes the cervix (the lower part of the uterus that extends into the upper end of the vagina) and surrounding tissue — is removed. The healthy uterus (located above) is preserved and reattached to the vagina (located below).
During the Operation–Using either minimally invasive or traditional “open” surgery, the surgeon removes the cervix and some of the pelvic lymph nodes. If the edge of the cervical tissue closest to the uterus is free of cancer cells, only the cervix is removed, rather than the entire uterus. The remaining portion of the uterus is left intact and is sutured to the vagina, creating a new cervix.
Our multidisciplinary team will devise a treatment strategy for you based on the stage of the cervical cancer, the size of the tumor, the surrounding tissues that may be affected, and whether the cancer has spread to other parts of the body. We also take into consideration your age and whether you wish to have children.
If you are a woman of childbearing age with early-stage cancer and you think you may wish to become pregnant at some point, our doctors can in many cases offer you a novel surgical approach called fertility-sparing radical trachelectomy.
During a radical trachelectomy, the surgeon starts with either a minimally invasive surgery (laparoscopy) or an open, traditional surgery to identify and remove the sentinel lymph node. A pathologist will then test the sentinel lymph node for cancer. If it is cancer-free, only partial removal of the cervix is needed, thereby avoiding the need to remove the entire uterus. This preserves the ability of a woman to conceive a child in the future, with delivery by cesarean section.
Due to refinements made by our surgeons, radical trachelectomy can be an effective way to remove early-stage cervical cancer without compromising your outcome.

The “Cerclage” Suture–Once the cervix and uterus have been separated, a suture (called a cerclage) is added where the newly created cervix and vagina will join. This suture helps to strengthen the cervix.

After the cerclage suture is added, the uterus is sutured back to the vagina, and the reproductive tract continues like normal. If the patient becomes pregnant after the surgery, she would be able to have a full-term pregnancy and give birth by cesarean section.
If you are a woman of childbearing age with early-stage cancer and you think you may wish to become pregnant at some point, our doctors can in many cases offer you a novel surgical approach called fertility-sparing radical trachelectomy.
RADIATION THERAPY & CHEMOTHERAPY FOR CERVICAL CANCER
We treat many cases of cervical cancer with surgery alone. However, there are women with disease that has started to spread, or who have tumors with high-risk features, for which we recommend additional measures such as radiation therapy and/or chemotherapy, a systemic treatment that kills cancer cells nearly everywhere in the body.
Treatment for Newly Diagnosed Disease
If your cancer has spread beyond the cervix and into surrounding pelvic tissues, our doctors may recommend that instead of undergoing surgery, you receive radiation therapy combined with chemotherapy. We may also recommend this combination if you have certain high-risk disease features at the time of your surgery that suggest an increased risk of the cancer returning, such as cancer cells in your lymph nodes or in parts of the tissue that is being surgically removed.
When radiation and chemotherapy are recommended in place of surgery, our doctors typically combine external-beam radiation therapy with internal radiation therapy. External-beam radiation therapy consists of x-ray treatments given daily for about five weeks. Low doses of chemotherapy drugs such as cisplatin (Platinol®) are used during this treatment to sensitize the cancer cells to radiation therapy.
Internal radiation is then given using high-dose brachytherapy, in which high doses of radioactive material are applied through a specialized applicator directly to the tumor. Studies have shown that this combined action can dramatically lengthen life in women with advanced cervical cancer.
Specialized approaches to external-beam radiation therapy may include the use of intensity-modulated radiation therapy (IMRT) as well. IMRT is a type of external-beam radiation that enables the doctor to customize the intensity of each radiation beam to conform to specific tumor shapes and sizes. IMRT not only reduces the dosage of radiation to healthy tissues but may also lessen your risk for side effects.
TREATMENT FOR ADVANCED OR RECURRENT CANCER
If your cancer has spread beyond the pelvis and into organs such as the lungs or liver, or you have recurrent disease, we will work with you to reduce your cancer-related symptoms and help you maintain your quality of life.
We primarily recommend chemotherapy for women with advanced or recurrent disease. Several drugs, such as cisplatin (Platinol®) and paclitaxel (Taxol®), are available. investigators are researching additional chemotherapy strategies that may be effective for patients.
 Some women with recurrent cervical cancer choose to undergo an involved surgery known as pelvic exenteration. With this approach, surgeons remove cancerous tissue and reconstruct the remaining organs to preserve as much function as possible.
Some women with recurrent cervical cancer choose to undergo an involved surgery known as pelvic exenteration. With this approach, surgeons remove cancerous tissue and reconstruct the remaining organs to preserve as much function as possible.
Brachytherapy can be done at the same time. We reserve this radical procedure for women who have otherwise limited treatment options.
ADMISSION
On the day of your operation you will be admitted to the Theatre Direct Admission area or into the the surgical Wards.A relative or friend can stay with you in the TDA area, while you wait. When you have gone to the theatre, your possessions will be taken to the main Gynaecology Ward and put into the bed space allocated to you. You will be brought back to the ward after your operation
PREPARATION FOR YOUR OPERATION
You will need to have a bath or shower in the morning, before coming into hospital, as discussed at your Pre-operative Assessment appointment.
While you are in the TDA area you will be visited by the following people:
A Doctor, who will visit you to see if you have any last minute questions about your operation. If you did not sign a consent form at the Pre-operative Assessment clinic this will now be done with you. The consent form should clearly state what operation you are having, the potential benefits and the risks involved. Please read the form carefully before signing it. You will be given a copy to keep.
The Anaesthetist, who will see you to discuss what type of anaesthetic you will have, and the different ways of controlling your pain after the operation.
A Nursing Assistant, who will record your blood pressure, pulse, breathing and temperature
- Ask you for a urine sample and check this for any abnormalities.
- Measure your legs for anti-embolism stockings. These stockings help to prevent blood clots from forming in the veins in your legs (known as DVT or deep vein thrombosis).
- You will wear the stockings for the operation and throughout your hospital stay. However, it is still important that you begin to move your legs and ankles as soon as you can after the operation, to help increase the blood circulation.
- Give you a theatre gown to put on, to wear for the operation complete a safety checklist with you, to make sure you are correctly prepared for your operation.
- You will not be able to eat or drink anything for a number of hours before your operation.
- The nurse at your Pre-operative
Assessment appointment will have explained when you should stop eating and drinking.
The Nursing Assistant in TDA will let you know whether your position on the operating list has changed and if you can have anything to drink after you have seen the Anaesthetist.
You may be given some tablets to take before your operation (such as painkillers and anti-sickness medication). The nurse will explain what the tablets are for.
A Nursing Assistant will then go with you to theatre and will stay with you until you have been handed over to the theatre staff in the anaesthetic room. If you have any further questions whilst you are in TDA, please talk to a member of nursing staff
AFTER THE OPERATION
You will stay in the recovery area, where you will be carefully monitored until you are well enough to go back to the ward. You may have an oxygen mask over your mouth and nose, which will help the effects of the anaesthetic to wear off The nurse will frequently monitor your blood pressure, pulse, breathing, oxygen levels and temperature. The nurse will also look at your wound dressing and will check your sanitary towel for any vaginal bleeding You may have a tube called a ‘wound drain’ coming out of your
tummy, to drain the fluid which collects after the operation.The tube is connected to a bag or bottle and normally needs to stay in for a day or so. The doctors will decide when it can be removed, and one of the nurses will take it out whilst you are on the ward. This may be uncomfortable, so we will offer you painkillers before it is removed have a choice of tablets, suppositories, or liquid painkillers, to help control any pain you may have.
You will be encouraged to take painkillers, as being comfortable helps to speed up your recovery.You may get wind pains a few days after the operation, which can be uncomfortable and make your tummy feel bloated. This should not last long and can be relieved with medicines, drinking peppermint tea, eating, and walking about. Eating and drinking
The anaesthetic may make you feel sick. If this happens we can give you tablets or injections that will help. You may also find that drinking straight after your operation makes you feel sick. You may be more comfortable starting off with a mouthwash or small sips of water.
You will have a drip going into one of your veins, which will make sure you get enough fluids if you are not able to drink.
When you are drinking enough fluids and no longer feel sick, the drip will be removed. We will tell you when you can start to eat. Passing urine
During the operation the doctors may put in a urinary catheter;
this is used to monitor the amount of urine you are producing. A catheter is a thin flexible tube that goes into your bladder, so that your urine can drain into a bag by the side of your bed. The nurses will check this regularly.
The catheter is usually removed the day after the operation.
If you do not have a catheter, the nurses will help you to use a bedpan, or will help you out of bed to use a commode (a portable toilet) until you are able to walk to the toilet yourself.
BOWELS
It may take two to three days before you have your bowels open. If you are having difficulty, we can give you some medicine to help. You will also find it helps if you:
- Drink lots of fluid.
- Eat a high fibre diet (e.g. wholemeal or granary bread, fruit, vegetables, cereals).
- Keep having short walks and moving around.
MOBILITY AND EXERCISES
On the first day after your operation you will be encouraged to sit out of bed in your chair, even if only for short periods of time.When you are in bed it is also important for you to continue to regularly move yourself around, to relieve pressure on your heels and bottom. You will be expected to move yourself, but the nurses will show you how and give you help if you need it.
We will also encourage you to rest, but it is also important to start doing exercises as soon as you can, to help you to recover.The important exercises that you should do are:
FOOT EXERCISES
Why? – To increase the blood circulation in your legs and help
prevent DVT (blood clot in the leg).
How do you do them? With your legs straight, briskly circle
or bend and stretch your feet up and
down from the ankles, 10 times.
How often? Every hour until you are up and fully
able to walk around.
BREATHING EXERCISES
Why? – After an anaesthetic, deep breathing can help to move any
phlegm (thick mucus) from your throat or lungs.
How do you do them? – Sit comfortably, supported with pillows
and with your knees bent. Take a long,
slow breath in through your nose and
hold for a count of two. Slowly sigh the
air all the way out. Repeat 3 times.
How often? – Every hour until you are walking well and
have no phlegm.
MOVING IN BED
Why? – It is good for your circulation, it helps to
prevent pressure sores and it also helps
to move wind.
How? Always bend your knees before turning
or moving up and down the bed.
Place a pillow or towel between your
knees. Use a towel or pillow as a wedge to
support your tummy.
Avoid twisting – Move your body as a whole, keeping your
shoulders and hips in line.
To get out of bed Bend your knees and turn onto your side. Let your feet and legs drop off the edge of the bed. Push yourself up with your arms into a sitting position on the edge of the bed. Then sit on the side of the bed for a few minutes before standing up
GOING HOME
You will be discharged from hospital when your doctors say you are ready. This will be approximately 2-4 days after your operation, but may be longer, depending on your medical needs.
Try not to compare your recovery with other women on the ward, as everyone is different.
When the doctors have decided you are well enough to go home, we will aim to get you home early in the day, usually before 11.00am. Please consider this when arranging for a family member or friend to collect you.
GETTING BACK TO NORMAL
After two weeks you can gradually start to do more. By six weeks
you are likely to be back to normal activity, with the exception of
any work involving heavy lifting or prolonged or vigorous sports.
As a general rule, listen to your body and use your common
sense. Do not push yourself too hard.
Cervical cancer surgery Follow up care
we are dedicated to helping cervical cancer survivors live their lives to the fullest after treatment. We offer comprehensive follow-up care for women who have been treated here as part of our institution-wide Survivorship Initiative.
Your follow-up care is provided by a nurse practitioner who specializes in the care of cervical cancer survivors. In addition to monitoring for signs of cancer recurrence, she focuses on identifying, preventing, and controlling any long-term and late effects associated with cancer and its treatment.
A visit with the nurse practitioner includes the following:
- Review of your recent medical history and a physical examination
- Assessment to detect recurrence of cancer
- Identification and management of the effects of cancer and its treatment
- Screeningreferrals for other cancers
- Health promotion recommendations related to nutrition, exercise, and smoking cessation
- Treatment summary and follow-up care plan
- Consultation with your physician as needed
Living Beyond Cervical cancer
We know that even after you’ve finished your cancer treatments, you may still need our help. We’re committed to supporting you in every way we can — physically, emotionally, spiritually, and otherwise — for as long as you need us.
We’ve built a program designed for cancer survivors and their families. Our Survivorship Center has many services for you and your loved ones, including support groups, follow-up programs, educational resources, and more.
Plus, our Resources for Life After Cancer program offers individual and family counseling, lectures and support groups, and practical guidance on employment and insurance issues, among other services. Visit the Survivorship Center to learn more.
REHABILITATION & EXERCISE
Cancer treatment can sap your strength, flexibility, mobility, and endurance. The experts at our centre can teach you therapeutic exercises and training programs that can help you heal. The state-of-the-art facility is specially tailored to the needs of people who’ve undergone treatment for cancer.