Ovaries are the female gonads — the primary female reproductive organs, each about the size of an almond. The ovaries lie on either side of the uterus against the pelvic wall in a region called the ovarian fossa. They are held in place by ligaments attached to the uterus.
reproductive organs, each about the size of an almond. The ovaries lie on either side of the uterus against the pelvic wall in a region called the ovarian fossa. They are held in place by ligaments attached to the uterus.
These glands have three important functions: they secrete hormones estrogen and progesterone, they protect the eggs a female is born with and they release eggs for possible fertilization.
Ovarian cancer is when abnormal cells in the ovary begin to multiply out of control and form a tumor. If left untreated, the tumor can spread to other parts of the body.
- Ovarian cancer rarely has noticeable symptoms when it is in its earliest stages. As the cancer progresses, subtle symptoms begin to appear, but they still may not be noticed right away, or they may be blamed on other common conditions, such as constipation or an irritable bowel.The symptoms of ovarian cancer include:
- abdominal bloating or swelling
- pain in the abdomen or pelvis
- difficulty eating, or feeling full quickly
- lack of appetite
- feeling an urgent need to urinate
- needing to urinate frequently
- change in bowel habits (constipation or diarrhea)
- change in menstrual periods
- vaginal bleeding between periods
- back pain
- weight gain or loss
Although the symptoms of ovarian cancer may be vague, particularly in the early stages, they are usually fairly constant and represent a change from how you normally feel. Symptoms also worsen as the cancer progresses.
If you experience any of these symptoms every day, or almost every day, for more than two to three weeks, speak with your doctor and specifically ask if you could have ovarian cancer. If it is ovarian cancer, the earlier we can diagnose it, the better the chances for an effective treatment.
There is no way to guarantee that you won’t develop cancer in your ovaries, peritoneum (a layer of tissue that lines your abdomen), or fallopian tubes. Most women have an approximately 1 in 70 chance of being diagnosed with one of these three cancers at some point in their lives. Aging is one risk factor; average age at diagnosis is 62.
Being aware of your risk level can help you make more-informed decisions about what to do to protect yourself and other family members.
Approximately 5 to 10 percent of women diagnosed with ovarian cancer have inherited an increased risk for the disease, which means that the cancer runs in the family. Risk is increased if a blood relative such as a mother, sister, grandmother or aunt has had ovarian cancer.
You are at a risk level near that of the general population if you have:
- no family history of breast or ovarian cancer
- a personal history of breast cancer diagnosed at age 41 or older
- no Ashkenazi Jewish heritage (individuals of Eastern European Jewish descent)
- a history of infertility and/or use of assisted reproductive therapies, such as in vitro fertilization (IVF)
- a history of endometriosis (a condition in which tissue from the lining of the uterus grows outside of the uterus)
- a history of hormone replacement use for the management of symptoms related to menopause
You are at increased risk if you have:
- a family history of ovarian or breast cancer
- a personal history of breast cancer prior to age 40
- a personal history of breast cancer diagnosed prior to age 50 as well as one or more close relatives diagnosed with breast or ovarian cancer at any age
- two or more close relatives diagnosed with breast cancer prior to age 50, or with ovarian cancer diagnosed at any age
- Ashkenazi Jewish heritage and a personal history of breast cancer prior to age 50
- Ashkenazi Jewish heritage and a first- or second-degree relative diagnosed with breast cancer prior to age 50, or with ovarian cancer at any age
You are at high risk — one in five or higher — if you inherited certain mutations in genes that are involved in cell growth, division, and DNA repair:
- the BRCA1 or BRCA2 genes (relative risk for ovarian cancer is greater than six times that of the general population)
- a mismatch repair gene mutation associated with a hereditary cancer syndrome known as Hereditary Non-Polyposis Colon Cancer (HNPCC)/Lynch syndrome
Other factors that can generally increase risk for ovarian cancer include:
- early menstruation or late menopause
endometriosis, a condition that involves tissue from the lining of the uterus growing outside the organ
In addition to the basics of following a healthy lifestyle by eating well, staying active, and maintaining your target weight, factors that may lessen the risk for ovarian cancer include:
- Pregnancy. The more full-term pregnancies a woman has had, the lower her risk of ovarian cancer.
- Oral birth control. The longer a woman takes birth control pills, the more she’s protected against developing ovarian cancer. This protection appears to last for many years after last taking the pill. However, because oral contraceptives also pose some risks, you should speak with your doctor for help in deciding if this is a good choice for you.
- Tubal ligation. Having your “tubes tied” may lower your risk for ovarian cancer, but experts emphasize that the procedure should be performed with the intention of preventing pregnancy — not reducing ovarian cancer risk.
Measures to Prevent Ovarian Cancer for Women at High Risk
Some women at high risk for ovarian cancer as a result of a family history decide to have surgery to remove the ovaries and fallopian tubes, in an effort to prevent the disease. The procedure, called salpingo-oophorectomy
Our genetics counselors may also recommend prevention strategies for women at high risk. Our surgeons are also investigating whether removing the fallopian tubes only, without removing the ovaries, may similarly reduce the risk of ovarian cancer.
Genetic Testing for Ovarian Cancer
Some women are born with an increased risk for developing ovarian, peritoneal, and fallopian tube cancer and doctors offer:
- hereditary risk assessment
- genetic counseling
- genetic testing
For example, you may wonder if you’re at increased risk because a family members related to you by blood has already been tested and found to carry the BRCA1 or BRCA2 genes associated with ovarian and breast cancer, or a blood relative may have been diagnosed with ovarian cancer, or diagnosed with breast cancer before age 50. Results of testing – which is done through a simple blood test – are usually available within a few weeks.
When you’re at Increased Risk
If testing indicates you’re at increased risk for ovarian cancer, one of our counselors can help you clarify and better understand the level of risk, and what your options may be for next steps. Together, we will help you make a plan for moving forward that is focused on your needs and what you are comfortable with.
Depending on your unique situation, options may include:
- a surgical procedure – salpingo-oophorectomy – in which surgeons remove your ovaries and fallopian tubes
- taking oral contraceptives to reduce risk
- regular and intensive screening with ultrasound (sonography) of the ovaries to detect abnormalities and monitoring levels of the marker CA125 in the blood
- fertility-sparing options
Salpingo- Oophorectomy ( Overy Removal Surgery)
Some women at high risk for ovarian cancer undergo a procedure called salpingo-oophorectomy to remove the ovaries and fallopian tubes as a preventive measure, before ovarian cancer has been diagnosed.
we can perform this procedure on an outpatient basis using a minimally invasive procedure known as laparoscopy. In this approach, a surgeon inserts a thin, tube-like instrument with a camera on its tip (a laparoscope) through the wall of the abdomen. Guided by the camera’s highly magnified image, we perform the operation through very small surgical openings (ports) using tiny instruments.
we can offer you a unique level of surgical care, with a team of ovarian cancer experts dedicated solely to women at risk for, or who already have, ovarian cancer. We perform more ovary removal surgeries than any other cancer center in the country.
No surgical procedure is without risks, but our team performs laparoscopy regularly, and our patients generally recovery very quickly. To minimize scarring, we can also often perform this procedure through a single incision in the belly button.
For most women, there is no effective way to screen for cancer in the ovaries, peritoneum (a layer of tissue that lines the abdomen), or fallopian tubes. Current tests are not reliable or accurate enough, especially for early-stage disease — and our experts have concluded that the risks generally outweigh potential benefits. This is one reason why it’s important for all women to be aware of the risk factors for this illness, and to stay sensitive to changes that might be symptoms of it.
For women at increased risk, we generally recommend screening with the following approaches at regular intervals:
- TRANSVAGINAL ULTRASOUND. Of the various imaging methods that have been evaluated for use in ovarian cancer screening, transvaginal ultrasound has consistently proven to be the most effective technique. With this approach, an ultrasound probe is inserted into the vagina to allow a radiologist or technician to view the organs in the pelvic region.
- BLOOD TEST FOR THE SERUM MARKER CA-125. Serum markers are substances in the blood that can be detected through blood tests. CA-125 is a protein produced by more than 90 percent of advanced epithelial ovarian cancers, the most common form of the disease. The CA-125 protein has become the most evaluated serum marker for ovarian cancer screening.
- Pelvic exam
Several studies have evaluated the combined use of transvaginal ultrasound and CA-125. These studies have suggested that the combination of these tests in the general population is not sensitive enough to detect early stage ovarian cancer. These tests also increase the rate of false positive results, which can lead to additional testing, anxiety and unnecessary surgery.
To check for ovarian cancer, your doctor will likely perform a pelvic exam to feel for lumps or changes in and around the ovaries and order additional tests if you’ve been experiencing persistent abdominal bloating, discomfort or other symptoms, or if you have risk factors for ovarian cancer.
Women found to have a suspicious mass or other indication of ovarian cancer should see an ovarian cancer specialist, ideally a gynecologic oncologist. The following tests and procedures can help determine if you have ovarian, fallopian tube, or peritoneal cancer (the peritoneum is a layer of tissue that lines your abdomen). They can also help in determining the stage of the cancer, and build a treatment plan specifically for you
Following a pelvic exam, we may recommend you undergo imaging tests such as transvaginal ultrasound, which is considered more accurate than a traditional ultrasound test because it allows technicians to place a special kind of wand called a transducer into the vagina and physically close to the ovaries. Sound waves emitted from the device bounce off organs within the pelvis to help identify growths and possible tumors.
Another commonly used imaging test to look for abnormalities is a CT scan of the chest, abdomen, and pelvis. A simple blood test to measure the level of the CA-125 protein can be helpful in making a diagnosis. This tumor marker can in some cases indicate the presence of ovarian cancer, since most epithelial ovarian cancer cells release this protein. However, because other types of tissue including non-cancerous tissues can also raise the level of this protein, the test isn’t usually recommended for women who aren’t experiencing symptoms, or who are at average risk for this cancer.
For many women, surgical procedures such as minimally invasive laparoscopy and robotic surgery are used to remove a sample of tissue for pathologists to determine if cancer is present. our surgeons often proceed with removing abnormal tissue and staging cancer if we find it.
By classifying ovarian cancer according to type and stage – from the earliest to the most advanced , doctors can prepare a treatment plan that’s customized specifically to your needs and condition. When learning about ovarian cancer, you may often see fallopian tube cancer and primary peritoneal cancer mentioned as well. This is because these three cancers are all treated the same way.
Stage I cancers of the ovary and fallopian tubes are considered early cancers. Stage II and higher are considered advanced ovarian, fallopian tube, and primary peritoneal cancers.
Fallopian tubes provide the path for eggs to travel from the ovaries to the uterus. The peritoneal cavity is the part of the abdomen that holds most of the abdominal organs, such as the uterus, liver, and spleen. The peritoneum is the lining of this cavity.
There are several types of ovarian cancer, which begin from these cell types:
- Surface epithelium, which involves cells that cover the ovaries’ lining
- Germ cells, which involve cells that will form eggs
- Stromal cells, which involve cells that release hormones and connect the different structures of the ovaries
After ovarian cancer is diagnosed, your doctor needs to know its stage to determine how far it may have spread. To do this, your surgeon will remove the tumor, as well as small samples of tissue from within the abdomen, including from the other ovary, fallopian tubes and peritoneum. (Your peritoneal cavity is where most of your abdominal organs are located.) These samples are sent to our laboratory for one of our expert pathologists to examine them for cancer cells with a microscope and with other tools.
Your doctor will then receive the pathology report, which lists the type of cancer that was found, the size of the tumor, if the cancer was contained within the ovary or if it had spread, the diagnosis, and the stage.
What are the four stages of ovarian cancer?
There are four stages of cancer of the ovaries, fallopian tubes and peritoneum, ranging from early to advanced cancer.
Stage I ovarian cancer is considered an early cancer.
This stage is divided into three substages, A, B, and C:
Stage IA: cancer cells are present in one ovary or fallopian tube.
Stage IB: cancer cells are present in both ovaries, or in both fallopian tubes.
Stage IC: cancer cells are present in one or both ovaries or fallopian tubes, and one of the following:
- The outside of the ovaries or fallopian tubes has cancer cells;
- The covering of the ovary, called the capsule, has broken open; or
- Cancer cells are found in your peritoneal cavity, its tissue lining, or fluid from your abdomen
- Stage II cancer has begun to spread. This stage is divided into two substages, A and B:
- Stage IIA: cancer has spread from the ovary or ovaries to the fallopian tubes and/or the uterus, or it has spread from the fallopian tubes to the ovaries and/or uterus.
- Stage IIB: cancer has spread in the peritoneal cavity to your bladder, colon, or rectum.
Stage III cancer is more advanced. This stage is divided into three substages, A, B, and C:
Stage IIIA is defined in one of two ways:
- cancer cells have spread to the closest lymph nodes, called the retroperitoneal lymph nodes.
- The surgeon cannot see the cancer with the naked eye, but using a microscope to examine the samples, the pathologist can see that the cancerous cells have spread to the outside the pelvis to the peritoneum (lining). The cancer may also have spread to nearby lymph nodes.
Stage IIIB: cancer inside the peritoneum can be seen by the surgeon, but is still 2 centimeters or smaller. The cancer has also spread outside the pelvis. It may have spread to nearby lymph nodes.
Stage IIIC: the cancer has grown to 2 centimeters in diameter or larger, and has spread to the peritoneum outside the pelvis. It may also have spread the outside of the liver and/or the spleen, as well as nearby lymph nodes.
Stage IV cancer is the most advanced form of ovarian cancer.
There are two substages, A and B:
Stage IVA: cancer cells are found in extra fluid that has built up around the lungs.
Stage IVB: cancer has spread to organs and tissues outside the abdomen, including lymph nodes in the groin.
Whatever type or stage your condition may be, doctors will find a way to build a treatment plan customized for you.
More than ever before, refinements in surgical techniques and how we care for women after surgery are improving outcomes for women at all stages of ovarian cancer. Our treatment approach for you will depend in large part on the stage of your cancer.
When diagnosed early, before it has spread (stage 1 disease), skilled surgery can lead to long-term survival in more than 90 to 95 percent of women. Some women at this early stage are cured by surgery alone, which is one of the reasons we’re so interested in finding reliable new ways to detect the disease at the earliest point possible.
Recent enhancements have also been made to chemotherapy regimens, such as intraperitoneal chemotherapy, and in finding immune system therapies.
Developing a Care Plan for You
As an
KIMS
patient, you will be cared for by a team of experts in surgery, medical oncology, pathology, and other areas, who meet regularly to discuss your treatment plan. Including specialists from different specialties – in addition to your one or two primary doctors – ensures that we consider all possible options for you, and that you receive the best possible care for your individual needs.
And as part of a comprehensive cancer center, at
KIMS
you and your family will have access to counseling and other supportive services.
Surgery is the main treatment for ovarian, fallopian tube, and peritoneal. It’s used for women with early and advanced disease, as well for women whose cancer has come back after treatment.
The type of surgery you receive depends on several factors, including the type and stage of your cancer, your general health, and whether you plan on having children in the future. Our doctors are experts at choosing the best surgical approach to treat your cancer while preserving your quality of life.
Laparotomy and Laparoscopy 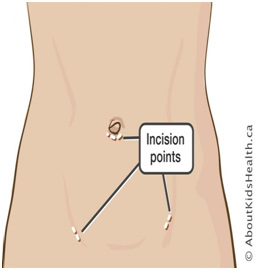
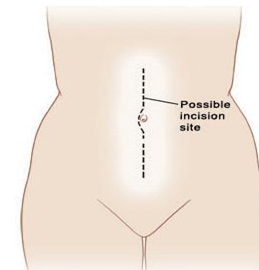
If you have early-stage ovarian cancer, meaning that the tumor is confined to the ovary and hasn’t spread, one option to remove the tumor is a traditional open surgery, called a laparotomy. A laparotomy involves making a relatively large incision in the abdomen.
In many cases, we recommend a minimally invasive laparoscopy procedure that’s done through smaller incisions.To perform laparoscopy, we insert a small video camera into the abdominal area through an endoscope (a device with a light at the end), and the surgical team guides the camera within the body. For early-stage tumors, you might have a laparoscopy done to:
- remove one of the fallopian tubes and ovaries along with the omentum, a thin fold of abdominal tissue that encases the stomach, large intestine and other abdominal organs. (This procedure is called an omentectomy.) Lymph nodes may also be removed.
- explore the abdomen for additional cancer and evaluate the extent of the disease
- drain any fluid buildup in the abdominal area
- retrieve small samples of abnormal tissue to perform a biopsy
- determine if you might benefit from debulking(removal of as much of the tumor as possible) and chemotherapy.
Robotic Surgery For Overian Cancer
Our specially trained surgeons often perform robotically assisted minimally invasive surgery to biopsy or treat early-stage ovarian cancer and, in some cases, recurrent ovarian cancer. To perform robotic surgery, the surgeon uses finger and foot controls, and the robot precisely copies his or her every movement. The surgical team at the bedside monitors you throughout the procedure, assisting as necessary. Studies suggest that if you have a robotic procedure with an experienced surgeon, you are likely to experience less postoperative pain, recover faster, and have good cosmetic results.
DEBULKING (CYTOREDUCTION) FOR STAGE IV OVARIAN CANCER
If your cancer has spread beyond the pelvis, surgeons will attempt to remove all the affected tissue during surgery. Depending on how much the cancer has spread, your surgeons may need to take out parts of the omentum, the diaphragm (the thin muscle below the lungs and heart that separates the chest from the abdomen), and segments of the bowel, the spleen, and parts of the liver.
With an approach called radical debulking, also known as cytoreduction, we remove as much cancerous tissue as possible to boost the effectiveness of chemotherapy in reaching and destroying cancer. The procedure usually involves removing the ovaries as well as the uterus, cervix, fallopian tubes, and any other areas containing diseased tissue. The goal is to leave no visible tumor behind.
If your cancer comes back (recurs), you may benefit from a second debulking operation, depending on how long the disease has been in remission and in what locations the cancer has returned.
PRESERVING FERTILITY
For certain younger women, we may consider an approach that preserves fertility by finding ways to keep a normal ovary intact, as well as the uterus. As long as the cancer is at a very early stage it’s sometimes possible to remove only the affected ovary (called unilateral oophorectomy) and fallopian tube, omentum, and lymph nodes preserving other pelvic organs necessary for fertility. Our surgeons are highly skilled in these methods to preserve fertility, as well as in knowing when such an approach might be right for you. The key consideration on our minds is always which technique is best for curing your cancer and giving you a normal life afterward.
SIDE EFFECTS OF OVARIAN CANCER SURGERY
Surgery for ovarian cancer can cause some pain and tenderness in the area where the operation occurred. These symptoms can usually be controlled well with pain medication. Symptoms of menopause, including hot flashes or vaginal dryness, also may arise soon after the surgery. These symptoms can usually be alleviated with specific therapies.
CHEMOTHERAPY FOR OVARIAN CANCER
To destroy any tumor cells that might be left behind after surgery for ovarian cancer, many women receive one form or another of chemotherapy, which works by interrupting the growth of cancer cells.
There are several ways to receive chemotherapy medicines for ovarian, fallopian tube, or peritoneal cancer:
• by mouth (oral chemotherapy)
• by injection into a vein
• as intraperitoneal chemotherapy placed directly into the lining of the abdominal area (the peritoneum) following surgery
we tailor the type of chemotherapy we recommend to each woman based on such factors as the type and stage of her cancer. We also make adjustments along the way as we assess whether the tumor is responding. Today we also have options that include targeted drugs, which are often effective in identifying and attacking cancer cells while basically sparing normal cells.
Targeted Therapies for Ovarian Cancer
While each type of targeted therapy works differently, all attack the inner workings of cancer cells – the so-called programming that makes them different from normal, healthy cells.
Targeted therapies for ovarian cancer include:
• Poly(ADP-ribose) polymerase (PARP) inhibitors, which are enzymes that function as key regulators of cell survival and cell death. Drugs that inhibit PARP-1 help fight cancers caused by mutations in BRCA1 and BRCA2. In December 2014, the PARP inhibitor Alaparib was approved for women with BRCA mutations who have experienced a recurrence of ovarian cancer.
• Bevacizumab (Avastin), a targeted therapy that has been studied frequently in ovarian cancer, and targets the blood vessels that supply the tumor and aid in growth.
Pazopanib (Votrient®), a targeted therapy drug that helps stop new blood vessels from forming. It has shown some promise in studies.
FOLLOW-UP CARE FOR OVARIAN CANCER
It’s one of our priorities to continue to check in with you once your active treatments are over to be sure you’re healing well and managing any side effects, and to watch for any signs that your cancer is returning.
We offer comprehensive follow-up care for people who’ve been treated here as part of our institution-wide Survivorship Initiative.
A nurse practitioner who specializes in the care of ovarian cancer survivors may work with your physicians to provide your follow-up care. In addition to monitoring you for signs of cancer recurrence your team will focus on identifying, preventing, and controlling any long-term and late effects associated with your treatment.
During a survivorship follow-up, we may:
• perform a physical exam and review your medical history
• complete an assessment to detect recurrence of cancer
• identify, evaluate, and manage any long-term or late effects of cancer and its treatment (both physical and psychological)
• discuss methods to prevent new health problems and make health recommendations related to nutrition, exercise, and quitting tobacco use
• recommend appropriate cancer screening or genetic testing for other cancers
In addition to working closely with your treatment team, we can provide a treatment summary and Survivorship Care Plan to you, your primary care doctor, and other medical providers. Your physicians can then incorporate this information into your overall medical plan. After each visit, we will update your other medical providers.
As your need for these follow-up visits decreases, we may recommend that you shift your care to your primary care doctor or gynecologist.
Living Beyond Ovarian Cancer
we know that even after you’ve finished your cancer treatments, you may still need our help. We’re committed to supporting you in every way we can — physically, emotionally, spiritually, and otherwise — for as long as you need us.
We’ve built a program designed for cancer survivors and their families. Our Survivorship Center has many services for you and your loved ones, including support groups, follow-up programs, educational resources, and more.
Plus, our Resources for Life After Cancer program offers individual and family counseling, lectures and support groups, and practical guidance on employment and insurance issues, among other services.