Mouth cancer is a type of head and neck cancer that begins on the lips or in the mouth.
It affects nearly 12.6 people in one lakh Indian population each year, and it is most closely linked to tobacco and alcohol use. Another name for mouth cancer is oral cavity cancer.
The term oral cancer refers to a broader range of cancers that includes those starting in the salivary glands and throat, as well as the mouth
Mouth cancer is most often diagnosed after your dentist notices symptoms during a routine exam.
Signs of cancer in the oral cavity include:
- a sore or lump on the lip or in the mouth
- a white and/or red patch on the gums, tongue, or cheeks
- unusual or persistent bleeding, pain, or numbness in the mouth
- swelling that causes dentures to fit poorly or become uncomfortable
If the disease is diagnosed early, surgery performed by an expert in head and neck cancer is usually the main treatment. The prognosis is often very good.
Treatment for mouth cancer may also include radiation therapy, chemotherapy, or a combination of the two.
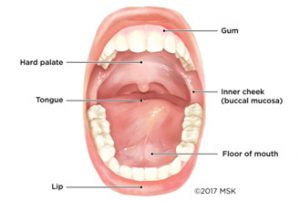
Cancer of the mouth can begin anywhere in the oral cavity, including the lips, floor of mouth, tongue, inner cheeks, hard palate (roof of the mouth), and the gums.
Mouth cancer can begin anywhere in the oral cavity. The oral cavity is another name for the mouth. It includes
- the lips
- the lining inside the cheeksand lips
- the front two-thirds of the tongue
- the upper and lower gums
- the floor of the mouthunder the tongue
- the hard palate(the bony portion of the roof of the mouth)
- the small area behind the wisdom teeth
The most common areas in the mouth where cancer develops are the tongue, the lips, and the floor of the mouth.
Cancer can also begin in other nearby areas, such as the back of the throat or the salivary glands.
What You Need to Know about Mouth Cancer
- Our surgeons’ primary goal is to cure the cancer while preserving your appearance and the function of your mouth.
- Radiation therapyis another important treatment for mouth cancer. We recommend radiation and chemotherapy in combination (called chemoradiation). They boost the effectiveness of treatment and achieve better outcomes when used together.
- Some people may require reconstructive surgeryas part of their operation to remove the cancer.
- Side effects of mouth cancer and its treatment can include problems with swallowing and speech. Some people experience limited range of motion in the jaw. Others develop problems with their teeth. Having experts in rehabilitation, speech pathology, dental oncology, and more is an essential part holistic approach to mouth cancer care.
- Tobacco and alcohol use are major risk factors for mouth cancer
Symptoms of mouth cancer include the following:
· Mouth ulcers that do not heal
A broken area of skin (ulcer) that will not heal can be a symptom of mouth cancer. Most people with mouth cancer have this symptom.
· Pain in your mouth
Pain or discomfort in your mouth that doesn’t go away is the other most common symptom of mouth cancer.
· White or red patches in the mouth or throat
An abnormal-looking patch could be a sign of cancer or precancerous changes.
- White patches are called leukoplakia.
- Red patches are called erythroplakia.
These patches are not cancer, but if left untreated, they may lead to cancer. A fungal infection called oral thrush can also cause red and white patches.
· Difficulty swallowing
Mouth cancer can cause pain or a burning sensation when chewing and swallowing food. Or you might feel like food is sticking in your throat. You may also cough or feel like food or liquid is going into the airway (windpipe).
· Speech problems
Cancer in your mouth can affect your voice. It might sound different. It may be quieter or husky. It may sound as if you have a cold all the time. Or you might slur some of your words or have trouble pronouncing certain sounds.
· A lump in your neck
You may have a lump in your neck caused by an enlarged lymph node. Swelling in one or more lymph nodes in the neck is a common symptom of mouth cancer.
Lumps that come and go are usually not due to cancer. Cancer typically forms a lump that slowly gets bigger.
· Weight loss
Weight loss is a common symptom of many different types of cancer. Mouth cancer can make it painful to eat and difficult to swallow, which can cause weight loss.
· Other signs of mouth cancer
These can include one or more of the following:
- a lump or thickening in your lip
- a lump in your mouth or throat
- unusual bleeding or numbness in your mouth
- loose teeth for no clear reason
- difficulty moving your jaw
Your mouth is composed of many different types of cells. The type of mouth cancer you have depends on which type of cells your cancer began in.
The vast majority of mouth cancers are squamous cell carcinoma. This is true regardless of where in your mouth the cancer begins.
Squamous Cell Carcinoma of the Oral Cavity
More than 90 percent of mouth cancers are squamous cell carcinoma. Squamous cells are thin, flat cells that look like fish scales. They are found in the tissue that forms the surface of the skin, the lining of the hollow organs of the body, and the lining of the respiratory and digestive tracts. Carcinoma means cancer.
Squamous cell carcinoma most commonly appears on parts of the body frequently exposed to the sun, such as the face, ears, and neck. But it also arises in the mouth.
Less common cancers of the oral cavity include:
Oral Verrucous Carcinoma
Verrucous carcinoma is a rare subtype of squamous cell carcinoma.
Oral Melanoma
Melanoma develops in the pigment-producing cells that give skin its color. Melanoma of the head and neck can occur anywhere on the skin or inside the nose or oral cavity. Lean more about melanoma treatment.
Where Mouth Cancer Begins
Even though most mouth cancers are squamous cell carcinoma, the treatment your doctor recommends depends on the exact location of the cancer. Learn more about the specific areas where mouth cancer can begin and the treatment options for each.
- Floor of Mouth Cancer
Often mistaken for a canker sore, floor of mouth cancer begins in the horseshoe-shaped area under the tongue.
- Gum Cancer
Often mistaken for gingivitis, gum cancer is highly treatable when found early.
- Hard Palate Cancer
It is rare for cancer to begin in the hard palate, but when it does the most common sign is an ulcer on the roof of the mouth.
- Inner Cheek Cancer (Buccal Mucosa Cancer)
Learn about the symptoms and treatment of inner cheek cancer, also called buccal mucosa cancer.
- Lip Cancer
Lip cancer is highly curable when diagnosed early. Learn more about symptoms, causes, and treatment for cancer that begins on the lips.
Tongue Cancer
Tongue cancer is a type of head and neck cancer that begins when the cells that make up the tongue grow out of control and form lesions or tumors.
There are two parts to your tongue, the oral tongue and the base of the tongue. Cancer can develop in either part. The oral tongue is the part you see when you stick out your tongue. This is the front two-thirds of your tongue.
The base of the tongue is the back third of the tongue. This part is very near your throat (pharynx). Cancer that develops in this part is classified as oropharynx cancer, or throat cancer.
Mouth cancer can affect anyone, but using tobacco products and regularly drinking too much alcohol greatly increase your chances.
Other major risk factors include sun exposure and tanning bed use. Infection with the sexually transmitted disease human papillomavirus (HPV) has been associated with mouth cancer as well, but there is a much stronger link between HPV and throat cancer.
Mouth Cancer Risk Factors
Tobacco
Studies have shown that as many as eight in ten people with mouth cancer are tobacco users. Tobacco includes both smoking and smokeless tobacco (snuff and chewing tobacco).
- Pipe smoking is a particularly significant risk for lip cancer, in the area where the lips touch the pipe stem.
- Smokeless tobacco is strongly linked with lip cancer, inner cheek cancer, and gum cancer.
- People who are exposed to secondhand smoke are at greater risk for mouth cancer.
If you smoke or chew tobacco, you can reduce your risk for mouth cancer — and the risk to those around you — by stopping now. If you’ve been diagnosed with mouth cancer or are in treatment, it’s not too late to quit.
Alcohol
Excessive consumption of alcohol is the other major risk factor for mouth cancer besides tobacco use. Most people who are diagnosed with mouth cancer drink heavily.
Tobacco and alcohol
The combination of tobacco and alcohol increases the risk for mouth cancer even further than either two risk factors alone. Studies have shown that people who use tobacco and alcohol together have a substantially greater risk for mouth cancer than people who don’t smoke or drink. According to the National Institutes of Health, nicotine and alcohol together account for around 80 percent of mouth cancers in men and around 65 percent of mouth cancers in women.
Betel quid and gutka
People who chew betel quid or gutka — which is more common in parts of Asia — have an increased risk of cancer of the mouth.
Gender
Mouth cancer is nearly twice as common in men as in women. This might be because men have higher rates of tobacco and alcohol use.
Age
Cancers of the mouth usually take many years to develop, so they are not common in young people. Most people are over 40 when cancer is first found in the mouth. The average age of diagnosis is around 60.
Ultraviolet light
Cancers of the lip are more common in people who spend time in the sun. Tanning beds use can also increase the risk for lip cancer.
Other risk factors
Other less common risk factors for mouth cancer include:
- a diet low in fruits and vegetables
- a weakened immune system
- graft-versus-host disease, a condition that sometimes occurs after a stem cell transplant
- lichen planus, a disease that often affects the skin
- certain genetic syndromes, such as Fanconi anemia and dyskeratosis congenital
Here are the top ways to reduce your mouth cancer risk:
- If you smoke or use other tobacco products, reach out to a tobacco cessation program, to get help quitting.
- If you drink alcohol, do so in moderation.
- Protect yourself against HPV infection by practicing safe sex.
- Do not use tanning beds and avoid extended periods of time in the sun.
It’s also important to schedule regular checkups with your dentist, particularly if you do use tobacco or drink heavily. That’s because many mouth cancers are found during routine dental appointments.
Finding mouth cancer early increases your chances for a cure and minimizes the impact of cancer on your quality of life.
Before you begin treatment, your care team will need to diagnose which type of mouth cancer you have. This is a key first step in developing the best treatment plan for you.
To start, your care team will take a complete medical history. They will want to know about any risk factors you may have, including your history of tobacco use and alcohol consumption.
If you have an ulcer or other possible signs of cancer, your doctor will ask you questions, such as when it developed and whether it has changed in size or appearance.
sophisticated pathology and imaging tests provide your care team with a great deal of information. The radiologists and pathologists who perform these tests not only focus on oncology but specialize in head and neck cancer. This training gives our team the expertise to ensure that you get the right diagnosis and to personalize your care as much as possible.
Throughout the course of your treatment, we’ll continue to use some of these tests to track the size of your tumor and assess your response.
Oral Tissue Biopsy
An oral tissue biopsy is the first step in diagnosing mouth cancer. During the biopsy, your surgeon removes a small amount of abnormal tissue from the area where mouth cancer is suspected. The tissue sample is then sent to a pathologist, who examines it under a microscope and works with the other members of your care team to make a diagnosis.
If surgery is part of your treatment, your pathologist will examine a sample of the tumor your surgeon removed to confirm the diagnosis.
we have a team of pathologists whose sole focus is diagnosing cancers of the head and neck. This specialization allows them to make the most precise diagnosis possible. A more precise diagnosis can improve the effectiveness of your treatment or spare you from treatment that won’t work against your disease.
Diagnostic Imaging for Mouth Cancer
As part of making a diagnosis, a radiologist will take special x-rays of your mouth, such as CT scans, MRIs, or Panorex. (A Panorex is an x-ray that shows the full upper and lower jaw, plus the sinuses.)
These imaging tests provide more details about the tissue. If cancer is found, the scans can show how deep the cancer is and if it has spread.
our radiologists use the most advanced imaging technologies to safely detect and monitor cancer. Their deep knowledge of mouth cancer allows them to choose the imaging approach that’s best for you and to define the precise extent of your tumor.
Genomic Testing for Advanced Mouth Cancer
Genomic testing is also called tumor sequencing or molecular profiling. It involves looking at the cells obtained from a biopsy to see if there are any genetic mutations (changes in your genes) that could be linked to the type of cancer you have.
Genetic information about your tumor can also help us predict the chances that your cancer will return after treatment.
Almost all of these genetic changes are found only in cancer cells, not in normal cells, which means they cannot be passed on to your children.
At some point, your doctor will tell you what stage of mouth cancer you have. Put simply, the stage describes how widespread or advanced the cancer is. Determining the stage helps doctors explain the extent of the cancer to you. It also helps them determine how to move forward with treatment, including surgery, radiation therapy, or chemotherapy.
Your doctor will assign a stage to your cancer after your physical exam and the initial results from your oral tissue biopsy or imaging tests. The stage may be adjusted if you have additional tests or after surgery. There are five stages of mouth cancer, starting at zero and going up to four. (They are represented by the Roman numerals I, II, III, and IV.)
These are the basic stages of mouth cancer:
Stage 0 Mouth Cancer
Stage 0 is also called carcinoma in situ, and this is the very beginning of the scale. It describes abnormal cells in the lining of the lips or oral cavity, which have the potential to become cancer.
Stage I Mouth Cancer
Stage I describes a very early stage of cancer. The tumor is not more than 2 centimeters, and the cancer has not reached the lymph nodes.
Stage II Mouth Cancer
Stage II describes a tumor that is larger than 2 centimeters but not more than 4 centimeters. Stage II cancer has not reached the lymph nodes.
Stage III Mouth Cancer
Stage III mouth cancer describes cancer that either is larger than 4 centimeters or has spread to a lymph node in the neck.
Stage IV Mouth Cancer
Stage IV is the most advanced stage of mouth cancer. It may be any size, but it has spread to:
- nearby tissue, such as the jaw or other parts of the oral cavity
- one large lymph node (more than 3 centimeters in size) and on the same side of the neck as the tumor, multiple lymph nodes of any size on the same side of the neck as the tumor, or one lymph node of any size on the side of the neck opposite the tumor
- distant parts of the body beyond the mouth, such as the lungs
Mouth cancer may be stage IV when it is first diagnosed. Stage IV mouth cancer can also be recurrent mouth cancer (cancer that has come back after treatment). The cancer may recur in the part of the body where it originally developed (regional recurrence), in the lymph nodes (regional relapse), or in another part of the body (called distant recurrence).
Stage III and stage IV cancers are more likely to recur than earlier-stage cancers.
Mouth Cancer Treatment
There are several ways to treat mouth cancer, depending on the location and stage, including:
- surgeryto remove the cancer
- radiation therapy, using high-energy rays (such as x-rays) to destroy cancer cells
- chemotherapy with drugs that kill cancer cells
Mouth Cancer Surgery
Surgery is the main treatment for most people with mouth cancer. Usually these tumors can be removed through the opening of the oral cavity, but some may require a more extensive approach. Which surgery is right for you depends on such factors as the size, stage, and location of your tumor.
head and neck surgeons place a strong emphasis on removing the cancer completely while preserving your quality of life. Achieving this delicate balance is our goal. It allows us to provide you with the best option for control of the disease while being highly attentive to your ability to speak, eat, and swallow.
Here you can find an in-depth overview about the different types of surgeries used to treat mouth cancer,.
- Glossectomy
- Mandibulectomy
- Maxillectomy
- Lymph Node Removal during Mouth Cancer Surgery
- Reconstructive Surgery for Mouth Cancer
- Dental Implants
- Mouth Cancer Surgery Recovery
Glossectomy
Glossectomy is the name of the surgery used to remove tongue cancers. For smaller cancers, only part of the tongue may need to be removed (partial glossectomy). For larger cancers, a more substantial portion of the tongue may need to be taken out.
Reconstruction of the tongue is often part of the care plan.
KIMS
’s plastic surgeons preserve and reconstruct the remaining portion of the tongue using innovative techniques to achieve the best function possible.
For example, they frequently perform a procedure called a radical forearm flap, taking skin from the forearm and the soft tissues underneath to rebuild the tongue. Using microsurgical techniques, they connect the tiny blood vessels and nerves from the forearm tissue to those in the neck. In addition, our plastic surgeons are able to provide sensation in the tongue and enhance a patient’s ability to speak and swallow by transplanting a sensory nerve from the forearm to the tongue.
Our speech and swallowing experts work closely with you before and after your surgery to design a personalized rehabilitation regimen. They are dedicated to making sure that you maintain as much function in your tongue as possible.
Mandibulectomy
A mandibulectomy (also called mandibular resection) involves the removal of part of the jawbone (mandible) when a tumor is very close or attached to the bone. A mandibulectomy is most common for mouth cancers that begin in the lower gums or the floor of the mouth.
The amount of bone that needs to be removed during a mandibulectomy varies according to the location of your tumor.
KIMS
’s head and neck surgeons use a combination of imaging and clinical expertise to make decisions about the need for, and the extent of, mandibular resection. They collaborate with radiologists who specialize in head and neck imaging to precisely define the extent of your tumor. This ensures that you get just the right amount of treatment.
In some cases, your surgeon may recommend removal of just a rim of the underlying jawbone. This is called a marginal mandibulectomy. The incision is covered with a graft of your own skin or the skin of a donor (an allograft). No reconstruction of the jawbone is needed, and it does not affect the shape of the jaw.
Other times, your surgeon may recommend that the full thickness of the mandible be removed. This is called a segmental mandibulectomy. At
KIMS
, our head and neck surgeons and plastic surgeons collaborate very closely to rebuild the jawbone. In some situations, they may use virtual surgical planning tools to fine-tune your operation.
we know that even after you’ve finished treatment for mouth cancer, you may still need our help. We’re committed to supporting you in every way we can — physically, emotionally, spiritually, and otherwise — for as long as you need us.
Maxillectomy
Maxillectomy is a surgery to remove bones that make up the hard palate (the bony front part of the roof of the mouth) or the nasal sinuses. It is most commonly recommended for mouth cancers that begin in the hard palate or the upper gums.
The space in the roof of the mouth that this operation creates can be addressed with either reconstructive surgery or a custom-fit obturator. Our team of head and surgeons, plastic surgeons, and maxillofacial prosthodontists collaborate closely to help patients decide which option is best for them, enabling them to speak and eat normally.
Lymph Node Removal During Mouth Cancer Surgery
Mouth cancers often spread to the lymph nodes in the neck first. Removing the lymph nodes in the neck (and other nearby tissue) may be done at the same time as the surgery to remove the mouth cancer. The goal of this procedure is to remove lymph nodes shown to contain, or that are likely to contain, cancer and to reduce the chance that the cancer may return in the future. Lymph node removal is most commonly recommended for cancers that begin in the tongue, the floor of the mouth, or the lower gums.
Our surgeons have extensive experience in performing these procedures and in preserving normal structures in the neck to leave minimal effects of surgery. They are currently testing a new optical-imaging approach allowing them to more precisely visualize cancer spread to lymph nodes. The noninvasive technique combines the use of nanoparticles acting as fluorescent probes with a handheld camera that detects light emitted by the particles, creating a high-resolution image showing cancer-cell location. Being able to detect where cancer cells have spread allows our surgeons to remove fewer nodes.
Reconstructive Surgery for Mouth Cancer
For many mouth tumors, your head and neck surgeon will close the wound with dissolvable sutures, or in some cases allow the wound to heal naturally. Other methods your surgeon may use include a skin graft, which uses your own skin (usually from the upper thigh) to repair the site, or an allograft, in which tissue from a donor is used.
For larger tumors, a plastic surgeon may repair the affected area using reconstructive techniques.
Reconstructive surgery for mouth cancer often involves the transplantation of tissue from one area of your body to the affected area of your mouth. Our goal is to preserve the form and functions of your mouth by using the latest techniques available.
Reconstruction for mouth cancer typically involves a microsurgical approach called free tissue transfer. This is when a plastic surgeon transfers a piece of your own tissue, along with the blood vessels, to the area where the cancer was removed in order to repair the surgical site. Tiny sutures (stitches) are used to connect the small blood vessels of the tissue to the blood vessels in the neck. That allows the transferred tissue to thrive and heal properly.
The type of tissue transfer you have depends on the size and location of your primary tumor. Areas we commonly transfer tissue from include the forearm, the fibula (the smaller of the two bones in the lower leg), the thigh, and the abdomen.
This table shows the types of tissue transfers most commonly recommended for mouth cancer patients, including where the tissue is taken from (the “donor site”) and which part of the oral cavity (the “recipient site”) the donor tissue may be used to reconstruct.
| Tytransfer | Donor site | Recipient site |
| Radial forearm flap | Forearm | Tongue, roof of mouth |
| Fibula free flap | Fibula (the smaller of two bones in lower leg), plus an artery, vein, and soft tissue | Jawbone |
| Anterolateral thigh flap | Thigh | Tongue |
| Rectus flap | Abdomen | Tongue, roof of mouth |
One of these is the fibula free flap approach. It is used to rebuild the jawbone after a mandibulectomy..
For people having reconstruction that involves the transfer of bone Our reconstructive surgeons use state-of-the-art virtual surgical planning software. This program (adapted from software used by architects) enhances the precision of your operation.
The software allows your doctors to develop a precise road map for your surgery. Your reconstructive surgeon works closely with your head and neck surgeon to make any fine adjustments and practice the details of your surgery together before your operation. This approach results in shorter, more precise operations with potentially fewer complications.
Some people may be offered the option of having dental implants as part of their care. Dental implants are metal posts that attach to the jawbone and are used to mount replacement teeth. For patients who choose to have dental implants,Our maxillofacial prosthodontists may be able to use innovative approaches to enhance your quality of life and speed the recovery process.
Radiation Therapy for Mouth Cancer
KIMS
has a team of radiation oncologists, including Nancy Lee, who specialize in the care of people with mouth cancers.
Radiation therapy for mouth cancer involves sending high-energy beams of particles (usually photons or protons) through the skin toward the tumor. When the beams reach the tumor, they destroy the cancer cells by damaging their DNA. Radiation therapy is known for its particular effectiveness against head and neck tumors, including cancers of the mouth.
Radiation therapy can be used in one of several ways for mouth cancers. It may be recommended after surgery to prevent the cancer’s regrowth. Radiation may also be used as the sole treatment if the tumor cannot be removed surgically or if the tumor regrows after surgery.
Why Choose for Mouth Cancer Radiation Therapy
-
KIMS
’s radiation therapy team has special training in caring for people with mouth cancer and works closely with the other members of your care team. -
KIMS
is the only center to offer weekly MRI imaging at no cost to patients. This mapping allows your radiation oncologist to optimize your radiation plan in real time. - You may be eligible to participate in clinical trials exploring new ways to boost the effectiveness of your treatment.
Types of Radiation Therapy for Mouth Cancer
There are many ways to treat mouth cancer with radiation.
KIMS
’s radiation oncologists specialize in head and neck cancers. They have extensive knowledge in knowing which approach will provide you with the most benefit.
KIMS
’s radiation therapy team has access to every modern form of radiation available. They will customize a treatment plan so precise that it factors in the size and shape of your tumor to the millimeter. Your team’s goal is twofold: to eliminate tumor cells and to prevent the side effects of treatment by keeping the healthy cells around the tumor safe.
Here you will find more in-depth information about the different approaches to mouth cancer radiation therapy.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-modulated radiation therapy combines the use of a highly advanced computer program with a metal device called a collimator. These tools allow your care team to shape the radiation beams to the exact dimensions of the treatment area.
Prior to the start of radiation therapy, a team of experts, including radiation oncologists and experienced medical physicists, collects detailed information about the treatment area. This includes:
- a CT scan to map the tumor in 3-D
- PET, CT, and MRI scans to generate an outline of the tumor
Your team then uses this information along with sophisticated treatment-planning software to calculate the optimal number of radiation beams and the exact angles of those beams. During treatment, the collimator is adjusted to produce the beams at the angles specified by the computer program.
This approach allows us to deliver more precise doses of radiation to the tumor while reducing the risk that healthy tissue is exposed.
Image-Guided Radiation Therapy (IGRT)
Image-guided radiation therapy uses imaging tests (CT, MRI, or PET) and special computer software to optimize the real-time delivery of radiation to the treatment area.
In this approach, daily imaging scans are performed to ensure an accurate position when the dose of radiation is delivered. The imaging scans are processed by special software to map changes in the tumor’s size or location. Your radiation therapy team can use this information to improve the accuracy of the radiation treatments while you are receiving them.
Adaptive Radiotherapy
In conventional radiation treatment planning, a team of radiation oncologists, radiation therapists, medical physicists, and dosimetrists works together to formulate your plan of care. Your team then carries out that plan during your course of treatment, which typically lasts six to seven weeks. Adaptive radiotherapy simply means that we repeat the planning process throughout treatment. Every time we detect certain changes that could affect the precision of the radiation, such as weight loss or tumor shrinkage, we review your treatment plan.
This personalized approach allows us to continually optimize your care while sparing healthy tissue. It is particularly beneficial for people who did not have surgery to remove a tumor.
Brachytherapy
Brachytherapy involves the placement of radioactive material in the body. The material is sealed inside a seed, pellet, wire, or capsule using a needle or catheter. The radiation given off by this source damages the DNA of nearby cancer cells. Brachytherapy is most commonly used for mouth cancer that has come back after prior treatment. Your doctors will discuss with you whether you are a candidate for brachytherapy.
Proton Therapy
Proton therapy is delivered by a device called a cyclotron. It sends a high-energy beam of protons through the skin toward the tumor.
Unlike photons, proton beams do not penetrate beyond the tumor. That’s the reason why proton therapy reduces the likelihood of side effects caused by damage to normal tissue. Because there could be fewer side effects, proton therapy allows us to use a higher radiation dose on the tumor, maximizing the chance of destroying it.
Proton therapy is extremely helpful for many people. At present, it is most commonly used for mouth cancer that has come back after prior treatment.
is one of a limited number of centers nationwide offering proton therapy.
Chemoradiation
Sometimes your doctor will recommend chemotherapy as part of your care plan. Chemotherapy can increase the sensitivity of your tumor to radiation treatment. The combination of radiation plus chemotherapy is called chemoradiation.
Cisplatin (Platinol®, Platinol®-AQ) is the most widely used and best studied standard chemotherapy drug used with radiation. Our researchers are studying other drugs that may be used in combination with radiation to further reduce the risk of your cancer returning. These options have different side effects that you may be better able to tolerate. We also think carefully about when to give chemotherapy — before, during, or after radiation. Our team carefully weighs each factor to ensure that we present you with the best strategy possible.
Clinical Trials
Clinical trials are research studies that test new treatments to see how well they work. People who choose to participate in a trial at
KIMS
receive the most advanced cancer treatment available, sometimes years before it’s offered anywhere else.
For mouth cancer, our researchers are studying immunotherapy, targeted therapies, and other approaches to boost the effectiveness of your radiation therapy. Learn more about clinical trials for mouth cancer.
KIMS
’s radiation oncologists work hard to minimize the side effects of treatment. They will explain to you in detail what to expect and when side effects are likely to occur.
The most common side effects of radiation to the oral cavity include:
- changes in your skin that look like a sunburn
- hoarseness
- changes in taste
- dryness of the mouth
- weakening of teeth
- pain, sores, or redness in the mouth
Our dental oncology team is available to support you with any problems that may arise with your teeth. They may also fit you with a custom mouth guard to protect your teeth during treatment.
Our rehabilitation team has extensive experience in helping people address the side effects of radiation therapy. A speech and swallowing specialist will meet with you before treatment to discuss any possible changes in your speech, voice, or swallowing. During and after treatment, they will provide you with exercises to prevent side effects. They will look out for any problems you are having with swallowing and make sure you are maintaining the range of motion in your tongue, jaw, and neck.
We offer comprehensive follow-up care tailored to the unique needs of head and neck cancer survivors. In addition to monitoring for signs that the mouth cancer has come back, we focus on identifying, preventing, and controlling any long-term and late effects associated with mouth cancer and its treatment
Rehabilitation
Speech and swallowing therapists are key members of the head and neck rehabilitation team. In addition, physical and occupational therapists help you improve your mobility after surgery or other treatments.
Our experts help you manage any changes in your speech and pronunciation, tongue or jaw range of motion, voice, or swallowing. They may also recommend
other tests to better assess your speech, voice, or swallow function. Your speech and swallowing therapist is involved in your care early after your diagnosis and works with you as long as you need, throughout treatment, recovery, and beyond.
Supportive care And Pain Management:
Our specialists in supportive care can help you cope with the side effects of therapy. These include pain, nausea, and fatigue. We can also help with the emotional and spiritual needs that often come up during and after cancer treatment.
If you are in pain during your treatments or even after they’re over, we have pain specialists who can help. We will build a plan that makes sense for you and your needs. Our experts can work with your doctor and pharmacists to give you solutions for both acute physical pain, which comes on suddenly, as well as chronic pain, which can linger. Our goal is to keep you as comfortable as possible.
Nutrition
Many people with mouth cancer have questions about diet and nutrition. Our food and nutrition team is trained in helping you understand and cope with a variety of conditions relating to cancer treatment.
Our expert dietitians provide medical nutrition therapy that can help you manage problems with swallowing, or changes in taste, your weight, and other issues. They work closely with your treatment team to customize a dietary plan that fits your own specific needs.