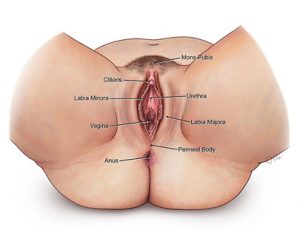
The vulva, which is part of a woman’s genitals, is at the opening of the vagina (birth canal). Vulvar cancer is classified based on the types of cells where it begins.
The vulva includes the following main parts:
Bartholin glands, which help lubricate the vagina during sex. One is on each side of the opening of the vagina.
Two skin folds around the opening of the vagina:
- Outer lips (labia majora), which are larger and have hair
- Inner lips (labia minora), which are small and do not have hair
Clitoris, which helps a woman feel sexual stimulation
Vulvar cancer is rare. Vulvar cancer usually grows slowly and may begin as precancerous changes that can be treated before they become cancer. The median age of diagnosis for Vulvar cancer is 68, and the disease’s five-year survival rate is about 71%.
Vulvar cancer causes & risk factors
Anything that increases your chance of getting vulvar cancer is a risk factor. These include:
- Age: More than half of women who develop vulvar cancer are over 70 years old.
- HPV (human papilloma virus)
- Smoking tobacco
- HIV (human immunodeficiency virus)
- Vulvar intraepithelial neoplasia (VIN), a precancerous condition usually caused by HPV
- Cervical cancer
- Melanoma or atypical moles on other parts of the body
- Family history of melanoma
Not everyone with risk factors gets vulvar cancer. However, if you have risk factors, it’s a good idea to discuss them with your health care provider.
Vulvar Cancer Symptoms
Symptoms of vulvar cancer vary from woman to woman. They may include:
- Red, pink or white bump (or bumps) with a rough or scaly surface on the vulva
- Burning, pain or itching in the genital area
- Pain when you urinate
- Bleeding and discharge when you are not having a menstrual period
- Sore on the vulva that does not heal for a month
- Change in a mole in the genital area
- Lump close to the opening to the vagina
These symptoms do not always mean you have vulvar cancer. However, it is important to discuss any symptoms with your doctor, since they may signal other health problems.
In rare cases, vulvar cancer can be passed down from one generation to the next.
The main types of vulvar cancer are:
Squamous cell, which is a wart-like growth. Verrucous vulvar cancer is a subtype. This cancer often can be treated successfully. It is the main type of vulvar cancer.
Adenocarcinoma usually starts in the Bartholin glands or sweat glands in the vulva. These make up about 8% of vulvar cancers. Paget disease of the vulva is a type of adenocarcinoma in which the cancer cells are in the top layer of skin.
Melanoma is a skin cancer that starts in cells that make pigment.
Sarcomas may be found in children as well as adults. These rare types of vulvar cancer start in the muscles or bones.
Vulvar Cancer Diagnosis
Early and accurate diagnosis of vulvar cancer is important. It also is crucial to find out if and where the cancer has spread. This helps your doctors choose the best therapies for you.
Specialized experts use the most modern and accurate equipment to diagnose vulvar cancer. With pinpoint attention to detail, our pathologists, diagnostic radiologists and specially trained technicians find the exact extent of disease. This helps increase the likelihood your treatment will be successful.
Vulvar Cancer Diagnostic Tests
If you have symptoms that may signal vulvar cancer, your doctor will examine you and ask you questions about your health, your lifestyle and your family medical history. Then, your doctor will do a pelvic exam and pap smear.
If you have a growth in the vulvar area that the doctor thinks might be cancer, the only way to tell for sure is a biopsy. Your doctor may use a special instrument called a colposcope to magnify the area and make it easier to remove the tissue. A small bit of tissue will be removed by:
- Excisional biopsy: A small knife is used
- Punch biopsy: A tiny punch tool is used
Other tests may help find out if you have vulvar cancer and if it has spread. These tests also may be used to learn if treatment is working.
Imaging tests, which may include:
- CT or CAT (computed axial tomography) scans
- MRI (magnetic resonance imaging) scans
- PET (positron emission tomography) scans
- Chest X-ray
In rare cases, vulvar cancer can be passed down from one generation to the next.
If you are diagnosed with vulvar cancer, your doctor will determine the stage of the disease.
Staging is a way of classifying cancer by how much disease is in the body and where it has spread when it is diagnosed. This helps the doctor plan the best way to treat the cancer.
Once the staging classification is determined, it stays the same even if treatment works or the cancer spreads.
Stage 0 (Carcinoma in situ): Abnormal cells are found on the surface of the vulvar skin. These abnormal cells may become cancer and spread into nearby normal tissue.
Stage 1: The tumor is confined to the vulva.
1A: The lesion is 2 centimeters or smaller and:
- Is confined to the vulva or perineum (the area between the anus and vagina)
- Has spread into the stroma 1 millimeter or less
- Has not spread into the surrounding lymph nodes
1B: The lesion is more than more than 2 centimeters in size and:
- Has spread 1 millimeter into the stroma
- Is confined to the vulva or perineum
- Has not spread into surrounding lymph nodes
Stage 2: The tumor is any size and has spread to adjacent perineal structures (anus, lower 1/3 of urethra, lower 1/3 vagina) but not to surrounding lymph nodes.
Stage 3: The tumor is any size and may or may not have spread to adjacent perineal structures. Cancer has spread to the lymph nodes.
Stage 4: The tumor has spread to other adjacent regions (upper 2/3 of the urethra, upper 2/3 of the vagina) or distant structures.
Our Approach to Vulvar Cancer Treatment
We concentrate on giving you the most-advanced treatments for vulvar cancer. Consideration for your quality of life is always a priority. For this reason, we focus on therapies that have the least impact on your body, yet target the cancer with the most-advanced methods.
Our physicians are at the forefront of pioneering less radical approaches, including sentinel node biopsy procedures. Research done here has helped the standard care for vulvar cancer evolve into less-radical surgery combined with other therapies, including chemotherapy and radiation.
We treat more women each year with this complex cancer than most oncologists in the nation. This gives us a level of experience and expertise that may lead to a higher chance for successful treatment in many cases.
And we’re constantly researching newer, safe, more-advanced vulvar cancer treatments. This translates to a number of clinical trials.
Vulvar Cancer Treatments
If you are diagnosed with vulvar cancer, your doctor will discuss the best options to treat it. This depends on several factors, including:
- The type and stage of the cancer
- Your overall health
- Your age
- Your preferences
Your treatment for vulvar cancer will be customized to your particular needs. One or more of the following therapies may be recommended to treat the cancer or help relieve symptoms.
Surgery
Vulvar cancer treatment usually includes surgery. Like all surgeries, vulvar cancer surgery is most successful when done by a specialist with a great deal of experience in the procedure.
The main types of surgery for vulvar cancer include the following:
Laser surgery: Lasers may be used to treat precancerous changes. Abnormal cells are burned off with a laser beam. Lasers are not used for invasive vulvar cancer.
Excision: The cancer and about a ½ inch of skin on each side of it are removed.
Vulvectomy: All or part of the vulva is removed.
Pelvic exenteration: In this complex surgery, the vulva and lymph nodes in the pelvis are removed. Depending on how far the cancer has spread, the lower colon, rectum, bladder, uterus, cervix and/or vagina may be removed.
If the bladder is removed, the surgeon will make a new way for your body to store and get rid of urine. It may be one of the following:
- Urostomy, which requires you to drain urine from a small opening
- A small plastic bag worn on the abdomen into which urine drains
If the rectum and lower colon are removed, the surgeon may be able to reconnect the remaining parts of the colon. If not, the colon is attached to the abdominal wall. Then feces pass through a colostomy (small opening on the outside of the body) into a small plastic bag on the front of the abdomen.
Inguinal lymph node dissection: Lymph nodes on one or both sides of the groin area are removed.
Sentinel lymph node biopsy: The surgeon removes the lymph nodes closest to they cancer and looks at them under a microscope. If the cells do not contain cancer, no more lymph nodes are removed. If the cells do contain cancer, other lymph nodes in the area will be removed.
Topical Therapy
This type of treatment may be used in precancerous vulvar cell changes. Medicine is applied to the growth. Drugs used include:
- Fluorouracil (5-FU), a chemotherapy drug
- Imiquimod
Chemotherapy
We offer the most up-to-date and advanced chemotherapy options for vulvar cancer.
Radiation
Radiation therapy sometimes may be given with chemotherapy to help make the cancer smaller before surgery. It also may be used to treat lymph nodes.
New radiation therapy techniques and remarkable skill doctors to target tumors more precisely, delivering the maximum amount of radiation with the least damage to healthy cells.