Colon cancer forms inside the large intestine, which is roughly five and a half feet long. The first five feet of the large intestine is called the colon. The rectum makes up the last six inches of the large intestine. Cancers found in the two organs are often grouped together as colorectal cancer.
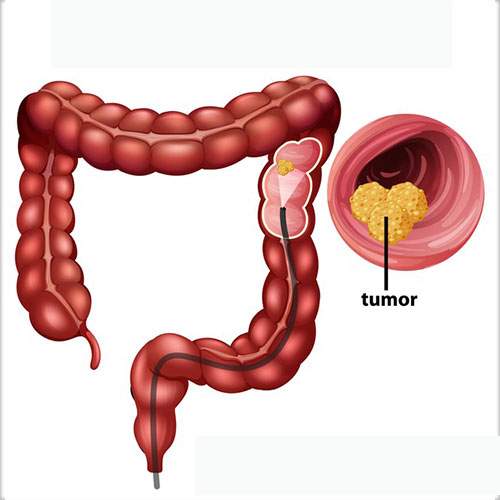
Colon cancer often develops slowly over several years. It typically starts as a small abnormal growth on the inner lining of the colon. This is called a polyp. Some polyps can eventually grow into cancer.
Colon cancer is often contained within the colon. But if left untreated, it can spread to other organs, most often the liver and lungs.
A small percentage of colon cancer is due to genetic causes that may be passed from parents to children.
Colon cancer forms inside the large intestine, which is roughly five and a half feet long. The first five feet of the large intestine is called the colon. The rectum makes up the last six inches of the large intestine. Cancers found in the two organs are often grouped together as colorectal cancer.
Colon cancer often develops slowly over several years. It typically starts as a small abnormal growth on the inner lining of the colon. This is called a polyp. Some polyps can eventually grow into cancer.
Colon cancer is often contained within the colon. But if left untreated, it can spread to other organs, most often the liver and lungs.
A small percentage of colon cancer is due to genetic causes that may be passed from parents to children. Colon cancer can be challenging to detect because you may feel only slight symptoms or even none at all. By the time you do feel symptoms, the cancer may be more advanced. For this reason, depending on your age, family history, and other risk factors, we may recommend regular screening for colon cancer.
What are the signs and symptoms of colon cancer?
These are symptoms you should not ignore because they may be signs of colon cancer:
- rectal bleeding or blood in your stool
- a change in your bowel habits, such as diarrhea, constipation, or narrow stool that lasts more than a few days
- unexplained abdominal pain or cramping
- a persistent urge to have a bowel movement that doesn’t go away after you have one
- unexplained weakness and fatigue
- unintended weight loss
- a diagnosis of anemia
- women who have bloating that doesn’t go away or happens with unexplained weight loss
Contact your doctor if any of these problems are severe or continue longer than you think they should.
If you have any rectal bleeding or blood in the stool, tell your doctor as soon as possible.
Signs and Symptoms of Colon Cancer in People under 45
If you are under 45 and have not been screened for colon cancer, it is particularly important that you do not ignore symptoms. The recommended age to begin colon cancer screening is now 45 years old. In recent years, there has been a troubling rise in colon cancer among people as young as their 20s and 30s who do not have a family history of the disease or typical risk factors.
Types of Colon Cancer
Most people who are diagnosed with colon cancer have a type called adenocarcinoma. There are other rarer tumor types too. These other types of colon cancer may be treated differently than adenocarcinoma. The section of this guide on the diagnosis and treatment of colon cancer refers primarily to adenocarcinoma.
Learn more about the types of colon cancer below.
Adenocarcinoma
The vast majority of colon cancer is adenocarcinoma. This is a cancer of the cells that line the inside surface of the colon.
Carcinoid Tumors
Carcinoid tumors start in hormone-producing cells in the intestines.
Gastrointestinal Stromal Tumors
Gastrointestinal stromal tumors can be a type of soft tissue sarcoma that can be found anywhere in the gastrointestinal tract but is rare in the colon. These tumors can also be other types of sarcoma that start in the blood vessels or connective tissue of the colon.
Lymphoma
Lymphoma is a cancer of the immune system. It more commonly starts in the lymph nodes but can start in the colon.
Hereditary Colon Cancer
About 5 to 10 percent of people get colorectal cancer because of specific mutations in the genes that are passed from parents to children, which are referred to as hereditary.
KIMS
’s colon cancer experts may offer you genetic testing to see if you have hereditary mutations in your genes that can increase your cancer risk. Whether you should have this testing is based on an assessment of your personal risk. Learn more about genetic testing for colon cancer and the types of hereditary conditions that often lead to the disease.
Understanding your risk factors for colon cancer can help you keep healthy habits and have more-informed discussions with your doctor about colorectal cancer screening.
You can control some risk factors for colon cancer but others you can’t.
What are the risks for colon cancer that I can control?
The following risk factors increase your chance of developing colon cancer:
- a diet high in red, processed, or charred meats
- a lack of exercise
- obesity, particularly extra fat around the waist
- smoking (studies show that smokers are 30 to 40 percent more likely to die of colorectal cancer)
- drinking too much alcohol
What are the risks for colon cancer that I can’t control?
Age
Most colon cancers occur after age 50 (unless there is a family history of the disease or a hereditary cause). However, in recent years there has been a troubling rise in colon cancer rates among people as young as their 20’s and 30’s.
Family History of Lynch Syndrome or Familial Adenomatous Polyposis
Some inherited disorders dramatically increase your risk of developing colon cancer. These include Lynch syndrome and familial adenomatous polyposis. Learn more about these and other inherited conditions that affect your risk of colon cancer as well as our genetic testing services.
History of Cancer
If you’ve had colon cancer before, you’re at an increased risk of having it again.
History of Inflammatory Bowel Disease
Inflammatory bowel diseases, such as ulcerative colitis and Crohn’s colitis, increase your risk of colon cancer.
Family History of Cancer
You have an increased risk of colon cancer if:
- a close family member, such as a parent or sibling, had colon cancer before age 50
- several blood relatives have had colon cancer
- there is a family pattern of certain other cancers, including endometrial, ovarian, gastric, urinary tract, brain, and pancreatic cancers
How can I lower my risk of colon cancer?
There are a number of risk factors for colon cancer. You can address some by changing your behavior but others you can’t change. Making healthier choices in your everyday life can help reduce many of these risks.
KIMS
recommends these healthy habits, which may lower your risk of colon cancer:
- Eat more fruits, vegetables, and fiber, and less animal and fat. The American Cancer Society recommends that you eat at least five servings of fruits and vegetables each day. Choosing such foods as beans and whole-grain bread, cereal, grain, rice, and pasta is a great way to improve your diet. Foods rich in calcium and folic acid (such as legumes, citrus, and broccoli) may also reduce your risk of colon cancer.
- Exercise regularly. Even moderate regular physical activity — such as taking the stairs instead of the elevator, raking leaves, or walking — can help reduce your risk of colon cancer.
- Maintain a healthy weight. Obesity is an important risk factor for colon cancer.
Does aspirin reduce the risk of colon cancer?
Some people who regularly use aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDS) may have a lower risk of colon cancer and polyps. Aspirin may also help prevent polyp growth in people who were previously treated for early-stage colon cancer or who previously had colon polyps removed.
You should only take aspirin under a doctor’s direction. Research suggests that not all people benefit. Also, NSAIDs can have serious side effects. Aspirin can cause stomach bleeding in some people, and drugs such as celecoxib (Celebrex®) may increase the risk of heart attack and stroke.
Does hormone replacement therapy reduce the risk of colon cancer?
Hormone-replacement therapy (HRT) consists of estrogen and progesterone. Women who use HRT after menopause may have a reduced risk of colon cancer. However, HRT can potentially cause other health problems. Talk to your doctor to learn more about the benefits and risks of HRT.
What is the average risk of colon cancer?
If you are age 45 or older, you are at an average risk of colon cancer if you have the following:
- no symptoms
- no personal or family history of colorectal cancer or precancerous polyps (noncancerous growths in the inside surface of the colon or rectum)
- no personal history of inflammatory bowel disease, such as ulcerative colitis or Crohn’s colitis
What is an increased risk of colon cancer?
If you have an increased risk of colorectal cancer, discuss with your doctor if you should have earlier, more frequent screenings.
You are at an increased risk if you have one of the following:
- a personal history of colorectal cancer or precancerous polyps
- a family history of a first-degree relative (such as a parent or sibling) who had cancer or precancerous polyps in the colon or rectum before age 50, or multiple family members with colorectal cancer or polyps
- a personal history of long-standing (more than eight years) inflammatory bowel disease, such as ulcerative colitis or Crohn’s colitis
- a family history of familial adenomatous polyposis (FAP). This condition is a rare form of hereditary colon cancer. FAP can lead to the development of hundreds or thousands of polyps in the colon at a very early age. If left untreated, people with FAP will almost always develop colon cancer by age 40.
- a family history of Lynch syndrome (formerly known as hereditary nonpolyposis colorectal cancer). This condition is caused by mutations in specific genes. It accounts for approximately 2 to 3 percent of all colorectal cancer diagnoses.
What should I know about family history and the genetic causes of colon cancer?
If you have more than one family member with colon or rectal cancer, or if you have a family member who had early-onset colorectal cancer (before age 50), your care team can help determine if you may be at risk of a possible hereditary condition that makes you more likely to develop cancer. If your care team feels that you may be at risk, we can refer you to our Clinical Genetics Service for further evaluation and customized screening options.
What if I have been treated for cancer before?
You may have an increased risk of colorectal cancer if you’ve had therapy for another type of cancer. In that case, your care team may recommend more frequent screenings.
What should I know about colon cancer if I am under age 45?
Real progress is being made against colon cancer, as more people are screened and treatment options improve. But in recent years there is a disturbing rise in colon cancer diagnoses in people under 50. Doctors and scientists are working to find out what’s behind this troubling trend.
What should I know about screening tests for colon cancer?
There are many types of colorectal cancer screening tests. Colonoscopy is the only test that can both find and remove small clumps of cells on the inner lining of the colon, called polyps. This means that a colonoscopy can both find and prevent colon cancer.
What is a colonoscopy?
A colonoscopy is a test in which a thin, flexible tube with a light and a video camera on its tip is placed in your colon to search for polyps. It’s the most effective way to find them. Your care team will prescribe a clear-liquid diet and medication to clear out your bowel during the 24 hours before the test. You’ll be sedated during the exam. Your doctor can usually remove any polyps that are detected, which then go to a pathologist (a doctor who specializes in diagnosing disease) for examination and analysis.
What is a flexible sigmoidoscopy?
A flexible sigmoidoscopy is similar to a colonoscopy. The main difference is that your doctor uses a shorter tube to examine the lower part of your colon.
What is a virtual colonoscopy?
A virtual colonoscopy (VC) is also known as a CT colonography. VC is an alternate screening option for some people. A radiologist uses CT scan technology to create 2-D and 3-D images of the colon. It does not require sedation. VC has limitations, however. For example, it requires the same preparation as a conventional colonoscopy: a clear-liquid diet and medication to clear out the colon. In addition, if VC detects a polyp or other abnormality in the colon, you may need a colonoscopy to remove it. VC can sometimes miss small or flat polyps.
What is a fecal occult blood test?
Because colon or rectal bleeding can be a possible sign of colon cancer, a fecal (stool) occult blood test may detect small amounts of blood in your stool that are not otherwise visible. The test works like this: For three consecutive days, you’ll place small stool samples on chemically treated cards. You’ll send those cards to a lab for testing. During this time, you have to follow a special diet to ensure that the test results are accurate. If an abnormality is detected, you may need to have a colonoscopy to remove it.
What is a fecal immunochemical test?
A fecal immunochemical test (FIT) screens for colon cancer by detecting blood in the stool. Unlike a fecal occult blood test, you don’t have to follow a special diet beforehand. FIT reacts to a part of the hemoglobin molecule (a protein found in red blood cells). If an abnormality is detected, you may need to have a colonoscopy to remove it. FIT is also called an immunochemical fecal occult blood test.
What is a stool DNA test?
A stool DNA test screens for cancer by looking for gene changes and blood in a stool sample. You do not need to follow a specific diet before submitting a sample. Like other stool tests, if an abnormality is detected, you may need to have a colonoscopy to remove it
Colon cancer is often found after symptoms appear. But most people with early-stage colon cancer don’t have symptoms. Those usually only develop with more-advanced disease. That’s why we recommend regular screening tests to detect and diagnose colon cancer at an early stage, when it’s easier to treat.
If you have symptoms that suggest you may have colon cancer, your doctor will take your medical history, perform a physical examination, and likely order diagnostic tests.
Colonoscopy and Biopsy for Colon Cancer Diagnosis
If we suspect that you have colon cancer based on those results, one of our specialists will do a colonoscopy and take a biopsy. In this test, the doctor removes a small piece of tissue with a special instrument. One of our expert pathologists (doctors who specialize in diagnosing disease) then examines the tissue sample under a microscope.
Your care team may recommend CT and MRI scans to determine the stage of the cancer and to see if it has spread to other organs.
Genetic Testing
Colon cancer can involve a number of genetic mutations that cause normal cells to become cancerous. These changes in the genes are called somatic mutations. They are found only in the cancer cells. They are not found in your normal cells, so they can’t be passed down to your children.
For some advanced cancers, pathologists at will do molecular testing on a tumor to find somatic mutations. These mutations can predict how a tumor might react to treatments. Knowing as much as possible about a tumor’s genetic makeup can help your care team choose the treatments that are most likely to help you.
If the cancer has spread outside the colon, your doctor will test biopsy samples for mutations in genes called EGFR, KRAS, and BRAF. These are common in colon cancer. We will also test for mutations in less common genes.
If your care team diagnoses you with colon cancer, the next step is figuring out the stage of the cancer, or how advanced it is. Staging helps us design a plan that treats you in the most effective way possible. So your care team can determine the stage of the cancer, you will have diagnostic tests to find out:
- how deeply the cancer has grown in the wall of your colon
- whether the cancer has spread to other parts of your body
The stage of cancer helps determine the typical treatment and outlook for people with cancer at that same point. However, each person’s cancer experience is unique.
What are the stages of colon cancer?
There are five stages of colon cancer, starting at zero and going up to four. They are often written with the Roman numerals I, II, III, and IV. In general, the lower the number, the less the cancer has spread.
What is stage 0 colon cancer?
Stage 0 colon cancer is found only in the innermost lining of the colon, called the mucosa.
What is stage I colon cancer?
Stage I colon cancer means that the tumor has spread beyond the inner lining but remains within the colon and has not spread to the lymph nodes. Lymph nodes are small organs that are part of the immune system and act like filters.
What is stage II colon cancer?
Stage II colon cancer extends through the thick outer muscle layer of the colon but has not spread to the lymph nodes.
What is stage III colon cancer?
Stage III colon cancer has spread outside the colon to one or more lymph nodes.
What is stage IV colon cancer?
Stage IV colon cancer has spread to other parts of the body, such as the liver or lungs. The cancer may be in the lymph nodes.
Which treatments are most likely to help you depends on your particular situation, including the location of your cancer, its stage and your other health concerns. Treatment for colon cancer usually involves surgery to remove the cancer. Other treatments, such as radiation therapy and chemotherapy, might also be recommended.
Surgery for early-stage colon cancer
If your colon cancer is very small, your doctor may recommend a minimally invasive approach to surgery, such as:
- Removing polyps during a colonoscopy (polypectomy). If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection. Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery). Polyps that can’t be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
Surgery is often the main treatment for early-stage colon cancers. The type of surgery used depends on the stage (extent) of the cancer, where it is in the colon, and the goal of the surgery.
Any type of colon surgery needs to be done on a clean and empty colon. You will be put on a special diet before surgery and may need to use laxative drinks and/or enemas to get all of the stool out of your colon. This bowel prep is a lot like the one used before a colonoscopy.
Polypectomy and local excision
Some early colon cancers (stage 0 and some early stage 1 tumors) and most polyps can be removed during a colonoscopy. This is a procedure that uses a long flexible tube with a small video camera on the end that’s put into the person’s rectum and eased into the colon. These surgeries can be done during a colonoscopy:
- For a polypectomy, the cancer is removed as part of the polyp, which is cut at its base (the part that looks like the stem of a mushroom). This is usually done by passing a wire loop through the colonoscope to cut the polyp off the wall of the colon with an electric current.
- A local excision is a slightly more involved procedure. Tools are used through the colonoscope to remove small cancers on the inside lining of the colon along with a small amount of surrounding healthy tissue on the wall of colon.
When cancer or polyps are taken out this way, the doctor doesn’t have to cut into the abdomen (belly) from the outside. The goal of either of these procedures is to remove the tumor in one piece. If some cancer is left behind or if, based on lab tests, the tumor is thought to have a chance to spread, a type of colectomy (see below) might be the next surgery.
Colectomy
A colectomy is surgery to remove all or part of the colon. Nearby lymph nodes are also removed.
- If only part of the colon is removed, it’s called a hemicolectomy, partial colectomy, or segmental resection. The surgeon takes out the part of the colon with the cancer and a small segment of normal colon on either side. Usually, about one-fourth to one-third of the colon is removed, depending on the size and location of the cancer. The remaining sections of colon are then reattached. At least 12 nearby lymph nodes are also removed so they can be checked for cancer.
- If all of the colon is removed, it’s called a total colectomy. Total colectomy isn’t often needed to remove colon cancer. It’s mostly used only if there’s another problem in the part of the colon without cancer, such as hundreds of polyps (in someone with familial adenomatous polyposis) or, sometimes, inflammatory bowel disease.
Colon cancer surgery can cure many people. However, some people develop undetectable microscopic tumor cells that eventually can become new tumors. These cells could spread to other parts of your body (metastasize).
Because of this, your care team may use adjuvant chemotherapy (chemotherapy given after primary therapy) to treat these microscopic cells. Chemotherapy is a drug or combination of drugs that kills cancer cells wherever they are in the body. For example, if you have colon cancer that has spread to your lymph nodes, chemotherapy is a standard treatment.
Chemotherapy for Metastatic Colon Cancer
Some standard chemotherapy drugs aren’t effective in colon tumors that have certain mutations. For people with cancer that has spread beyond the colon (metastatic colon cancer), we analyze the tumors to look for specific genetic mutations. Knowing about a tumor’s mutations can help determine which chemotherapy drugs will be most effective and minimize side effects.
If you have colon cancer that has spread to other organs, surgery to remove the tumor first may not be the best treatment option. As long as the tumor isn’t causing problems in your bowel, chemotherapy may be a better choice.
Having chemotherapy first has two potential benefits:
- You may be able to avoid the risk of surgical complications.
- You can start cancer treatment throughout your entire body without delay.
Colon cancer surgery can cure many people. However, some people develop undetectable microscopic tumor cells that eventually can become new tumors. These cells could spread to other parts of your body (metastasize).
Because of this, your care team may use adjuvant chemotherapy (chemotherapy given after primary therapy) to treat these microscopic cells. Chemotherapy is a drug or combination of drugs that kills cancer cells wherever they are in the body. For example, if you have colon cancer that has spread to your lymph nodes, chemotherapy is a standard treatment.
Chemotherapy for Metastatic Colon Cancer
Some standard chemotherapy drugs aren’t effective in colon tumors that have certain mutations. For people with cancer that has spread beyond the colon (metastatic colon cancer), we analyze the tumors to look for specific genetic mutations. Knowing about a tumor’s mutations can help determine which chemotherapy drugs will be most effective and minimize side effects.
If you have colon cancer that has spread to other organs, surgery to remove the tumor first may not be the best treatment option. As long as the tumor isn’t causing problems in your bowel, chemotherapy may be a better choice.
Having chemotherapy first has two potential benefits:
- You may be able to avoid the risk of surgical complications.
- You can start cancer treatment throughout your entire body without delay.

