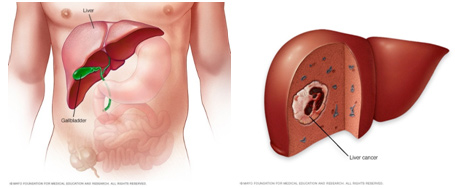
The liver is the body’s largest internal organ. It’s located below the right lung and divided into right and left lobes. The liver is made up of cells called hepatocytes that process nutrients in your blood. It’s responsible for breaking down and storing many of these nutrients, and it helps remove waste from the body. The liver also makes bile, which is a fluid that helps you digest food. It makes proteins that help stop bleeding from cuts or wounds too.
It’s more common to develop liver cancer that has spread from somewhere else in the body, which is called LIVER METASTASES. PRIMARY LIVER CANCER, which means the cancer begins in the liver itself.
The number of people with primary liver cancer is growing as more have conditions that affect the liver and increase the risk for cancer in this organ, such as chronic hepatitis C. Primary liver cancer tends to occur in people in their 60s and 70s, and is more common in men.
Liver cancer presents a special challenge because you may not notice any symptoms when the disease is starting and in its early stages. Doctors usually discover signs of liver cancer when screening people for an underlying liver condition, such as chronic hepatitis.
If you do have symptoms, they may include:
- yellowing of the skin and the whites of the eyes (jaundice)
- darkening of the urine
- lightening in the color of the stool
- an overall feeling of poor health or weakness
- loss of usual appetite and weight loss
- fever
- fatigue
- bloating
- swelling of the legs and abdomen
- generalized itching
- pain or discomfort in your abdomen
Speak with your doctor if you have any of these symptoms so that you can be sure to get a proper diagnosis and treatment if needed.
What are the main causes of primary liver cancer? Scarring of the liver (cirrhosis) caused by too much alcohol use or infection with hepatitis B or C infection are largely to blame.
Up to 80 percent of primary liver cancers around the world are caused by infection with the hepatitis B or hepatitis C virus. Infection with this virus can affect you for many years and result in cirrhosis (scarring) in your liver. People get infected through physical contact with the blood or bodily fluids of a person who has the virus in their body.
You can get infected with the hepatitis B or C virus through:
- unprotected sex
- sharing unsterilized needles
- a blood transfusion, if received before 1992 (after that year, donated blood has been screened for the virus)
Because primary liver cancer caused by viral hepatitis tends to develop slowly over the course of two to three decades, there are steps you can take to get screened for the infection and prevent it from becoming advanced.
Ways to Prevent Liver Cancer
You can lower your risk for developing liver cancer by following healthy lifestyle measures, such as regular exercise, controlling your weight, and eating a healthy diet with limited amounts of alcohol.It’s also important to avoid infection with the hepatitis B and C viruses.
Protect against Hepatitis B and C Infection
If it isn’t treated, hepatitis B infection can lead to cirrhosis (scarring), liver failure, and cancer. Vaccines for hepatitis B are available for children and adults. If you are at risk for hepatitis B or C infection, consider undergoing a screening test.
If you have chronic hepatitis B, you might be a candidate for antiviral therapy, which can slow down the progression of liver disease and decrease (although not eliminate) the risk of liver cancer. While there is no vaccine for hepatitis C, the right treatment can eliminate the virus in most people.
If you have chronic hepatitis, you should visit your doctors for regular surveillance with imaging tests, such as ultrasound, CT, or MRI.
Other Risk Factors for Liver Cancer
In addition to infection with chronic hepatitis B and C, the following conditions increase the risk of developing liver cancer.
- Nonalcoholic fatty liver disease (NAFLD): This disease is also called nonalcoholic steatohepatitis. It causes a type of fat called triglycerides to gather in the liver, which can lead to damage. NAFLD can cause cirrhosis (scarring of the liver) and liver failure. It commonly occurs in people who are overweight or obese, or who have type 2 diabetes or a metabolic syndrome characterized by high blood sugar, extra body fat around the waist, and abnormal cholesterol levels. With obesity on the rise in the United States, NAFLD is increasingly a risk factor for liver cancer.
- Cirrhosis of the liver made worse by alcohol use: Drinking alcohol greatly increases the risk of cancer in people infected with the hepatitis B or C virus, so it’s important to avoid drinking if you have viral hepatitis.
- Hemochromatosis: This is one of the most common genetic disorders. It increases the risk of liver cancer because it causes the body to absorb too much iron from food. Hemochromatosis is most commonly found in people of Irish descent.
- Exposure to arsenic: This naturally occurring substance is sometimes found in drinking water. It is also a part of vinyl chloride, a chemical used in making certain plastics that can increase your risk for liver cancer.
- Too much intake of male hormones or anabolic steroids: These hormones, which build muscle, are considered a risk factor.
- Ingestion of aflatoxin: Aflatoxin is generated by certain types of mold in improperly stored grains and nuts.
There are several types of liver cancer. Each type is different in the way it develops and changes over time, as well as in how it should be treated.
Hepatocellular Carcinoma
The most common type of primary liver cancer is hepatocellular carcinoma. This cancer begins in liver cells called hepatocytes, which process nutrients in the blood. It often develops as a single tumor that spreads to other tissues and organs over time.
Most people with hepatocellular carcinoma also engage in behaviors or have a disease of the liver that causes inflammation and scarring in the organ, such as:
- Long-term infection with the hepatitis B or C virus
- A metabolic abnormality, such as nonalcoholic fatty liver disease or too much iron in the body
- Excessive alcohol consumption
Intrahepatic Cholangiocarcinoma
Intrahepatic cholangiocarcinoma is the second most common type of primary liver cancer. It starts in the tube like structures called bile duct cells that deliver bile, a substance that helps in digesting food. This type of liver cancer tends to develop in people who have:
- Been infected with the hepatitis B or C virus
- Primary sclerosing cholangitis, a disease that can lead to inflammation and scarring of the bile ducts
- Nonalcoholic fatty liver disease, which involves inflammation that’s unrelated to alcohol consumption
Fibrolamellar-Hepatocellular Carcinoma (FLL-HCC)
Also known as fibrolamellar carcinoma, this rare type of hepatocellular carcinoma is less aggressive than other types of primary liver cancer. It usually develops in people in their 20s and 30s. It’s often misdiagnosed as a type of noncancerous liver tumor called focal nodular hyperplasia.
Angiosarcomas, Hemangiosarcomas, and Hemangioendotheliomas
These tumors develop along the inner linings of blood vessels. They almost only occur in very young children and are considered curable.
Hepatoblastomas
This type of primary liver tumor is made up of tissue that looks like fetal liver cells, bile duct cells, or mature liver cells when we examine them under a microscope. Hepatoblastomas are curable.
It’s very important to get an accurate diagnosis of primary liver cancer so that your condition can be treated the right way from the beginning.
Your diagnosis information is used to create a treatment plan that’s just right for you. Along with a diagnosis, we’ll determine the extent (stage) of your cancer through blood tests, diagnostic imaging, biopsy, and genetic testing of your tumor.
- A test that measures the level of a protein produced by the liver called alpha fetoprotein (AFP) can indicate that you have fibrolamellar-hepatocellular carcinoma.
Blood Tests
A test that measures the level of a protein produced by the liver
called alpha fetoprotein (AFP) can indicate that you have fibrolamellar hepatocellular carcinoma (FLL-HCC).
Diagnostic Imaging
Imaging tests help us learn about the exact location of your tumor and assess the condition of the organ and surrounding tissues and blood vessels. These tests also help guide our surgeons and interventional radiologists during procedures.
We commonly use CT scans and MRI to create detailed images that include the insides of areas of the liver, gallbladder, bile ducts, nearby lymph nodes, and other internal organs.
We can also use ultrasound tests to determine if the cancer is benign (noncancerous) or malignant (cancerous). A special kind of Doppler ultrasound can help us examine the veins where blood travels from your gastrointestinal tract and spleen to your liver. We can then see if the tumor has invaded these areas and caused a blood clot.
Biopsy
A biopsy is an important part of your diagnosis because it lets us know how extensive your tumor is and what types of cells it contains. At most institutions, liver biopsies are guided by ultrasound or CT imaging. we also have a unique interventional MRI and interventional PET/CT unit that uses minimally invasive techniques to help us in diagnose challenging cases.
To get more information about the extent of your tumor and the types of cells involved, we may do a fine-needle aspiration biopsy. In this test, a doctor inserts a thin needle into the liver to get a small tissue sample for one of our pathologists to examine under a microscope. Or your doctor may order a core biopsy, for which we use a slightly larger needle.
Your doctors may recommend a laparoscopy to get tissue samples for a biopsy. Laparoscopy can sometimes eliminate the need for surgery to make a diagnosis. With laparoscopy, the surgeon passes a thin, lighted tube with a camera on its tip (a laparoscope) through a small incision in the abdomen to inspect the liver and other organs.
Testing for Fibrolamellar-Hepatocellular Carcinoma (FLL-HCC)
To examine you for fibrolamellar-hepatocellular carcinoma, a biopsy is crucial because we learn about what cells are involved in the cancer. A biopsy can also help us determine if you have a combination of FLL-HCC carcinoma and another type of liver cancer called cholangiocarcinoma. This can guide us to the most effective therapy for you.
Genetic Testing of Tumors
Having information about the genetic makeup of your tumor can help us select the most effective therapies for you. Pathologists do this through laboratory tests they perform on liver tissue from a biopsy.
We’ll look for specific mutations in a number of genes. We know that tumors containing mutations in the genes KRAS and BRAF don’t respond well to a class of drugs called epidermal growth factor receptor inhibitors, for example, so our doctors know to start treatment with a different approach.
The stage of liver cancer you have refers to how far the disease has spread through your body. It’s possible that you’ll need additional tests to understand the stage of the tumor.
Information from staging tests can help us figure out whether:
- The tumor is in one area of the liver and can be removed
- The tumor is in one area but cannot be completely removed safely
- Cancer has spread throughout the liver or to other parts of the body
- Cancer has reoccurred in the liver or in another part of the body after it was eliminated with a first round of treatment.
We’ll determine the best treatment approach for you based on the stage of your disease. We also factor in whether you have other conditions that can affect the health of the liver, such as hepatitis, cirrhosis (scarring), or diabetes. If we find extensive cirrhosis or liver failure, for example, we may look to options other than surgery to treat your cancer.
The outlook for people with primary liver cancer has never been better. Today, many people survive the disease.
Our surgeons perform many of liver cancer procedures each year. They are often able to offer treatment to people whose tumors aren’t considered operable at other hospitals.
Because surgery for liver cancer can be challenging — many important blood vessels are near the liver — we may recommend chemotherapy, targeted therapy, or other approaches in addition to considering surgery. Sometimes we use radiation therapy to treat the disease, but this isn’t as common.
When surgery isn’t the best option, we may call on our interventional radiologists to perform minimally invasive techniques using CT, ultrasound, or MRI to guide the treatments directly to your liver and destroy the tumor. Our doctors are skilled in ablation, NanoKnife techniques, and embolization to get rid of liver tumors.
Treatment for Advanced Disease
Many people don’t have surgery for primary liver tumors because the cancer is too advanced at the time we find it, or they have an underlying liver disease, such as cirrhosis (scarring of the liver). Sometimes liver tumors are so small that it doesn’t make sense to have surgery, since other therapies are likely to be just as effective.
We’re constantly evaluating new targeted medications, either alone or combined with other drugs, to improve how we care for our patients. For many people, targeted agents don’t cause the side effects that are common for chemotherapy, such as fatigue, nausea, and diarrhea.
Often we’re able to offer patients participation in an investigational therapy for primary liver cancer through a clinical trial.
For people with fibrolamellar-hepatocellular carcinoma, our doctors may prescribe sorafenib (a commonly used targeted drug), or we may recommend a clinical trial exploring new treatment options. In some cases, clinical trials are available even if you have advanced cirrhosis or liver failure.
Can Liver Tumors Be Benign?
Benign (noncancerous) tumors can form in the liver. Usually they don’t cause symptoms and are only found by chance when a person undergoes imaging tests for another health condition.
We may recommend that benign liver tumors be treated if they cause bleeding, abdominal pain, or other major symptoms.
Our researchers are evaluating a variety of drugs, including new and experimental drugs, for their potential effectiveness in treating tumors with these and other mutations.
we can offer you a good chance that you’ll have a better outcome with liver cancer surgery than you would have elsewhere.
Liver surgery can be challenging because many of the important blood vessels leading to and from the heart pass by this organ. Also, the liver can tear easily, and it bleeds a lot if injured. Because our surgeons perform hundreds of liver cancer operations each year, we’re familiar with techniques that can limit blood loss and lessen the need for transfusions during surgery.
Surgery is often the best treatment for primary liver cancer when it’s at an early stage and hasn’t spread to nearby blood vessels. It’s also important that you don’t have underlying medical conditions, such as liver cirrhosis (scarring). Depending on your particular situation, we may recommend chemotherapy before surgery to help shrink your tumor first.
Interventional radiologists are in the operating room to assist with minimally invasive techniques for primary liver cancer, such as ablation, Nanoknife, or embolization if needed.
Because the liver is one of two organs in the body that can regenerate (regrow), we can remove as much as 80 percent of the organ, and it will rebuild itself within a matter of weeks, we use surgical techniques that leave large portions of the healthy part of the liver in place, reducing your risk for complications. In addition, our radiologists can perform a technique that redirects the blood supply to the healthy liver and stimulates cell growth before surgery.
Difficult Cases and Liver Transplantation
Our liver cancer surgeons are known for operating on primary liver cancers that other centers won’t attempt. For example, we’re experienced in managing cholangiocarcinoma, an uncommon cancer that arises from the bile duct cells.
Liver transplantation is an option for some people with primary liver cancer as well. This can be a smart approach if your tumors are small in size and number and haven’t spread to nearby blood vessels — and if you don’t have cirrhosis or another liver condition. Your team will let you know if this approach might be a good one for you, and they can coordinate with area hospitals to have the procedure done.
Ablation, NanoKnife®, and Other Minimally Invasive Techniques for Liver Cancer
When it comes to surgery, precision matters. We’re experienced in minimally invasive therapies involving imaging techniques — such as CT scans, ultrasound, and MRI — to guide the delivery of treatments directly to liver tumors. Our interventional radiologists help with this in the operating room.
When it’s an option that might work well for you, we’ll offer minimally invasive laparoscopic or robotic surgery to remove your tumor. Laparoscopic procedures involve inserting a laparoscope (a thin, lighted tube with a camera on its tip) through a tiny incision in your abdomen. This approach can remove tumors or, in some cases, part of the liver.
Our interventional radiologists are skilled in the following minimally invasive approaches to destroy liver tumors. These techniques can be used alone or in combination with other minimally invasive therapies before surgery or in addition to chemotherapy.
- Ablation destroys a tumor by cutting, vaporizing, melting, or using intense heat or cold.
- NanoKnife uses electrical currents to make holes in the cancer cells and eliminate them.
- Embolization, including chemoembolization, involves blocking or lessening blood flow to the main source of blood for liver tumors
Thermal Ablation for Liver Cancer
We usually recommend ablation only if you have three or fewer tumors. Using image guidance, we deliver the therapy through a probe and directly into the tumor.
There are several types of thermal ablation, including:
- radiofrequency ablation, which uses radio waves to superheat the tumor
- cryoablation, which freezes the tumor
Other types of thermal ablation use lasers, microwaves, and focused ultrasound waves to kill tumor cells.
Typically, we deliver these therapies using image guidance and don’t need to make a surgical incision. We can deliver the therapy through a laparoscope, for example, or in some cases during open surgical procedures. Whether we choose heat or cold depends on the size, location, and shape of your tumor.
Chemical Ablation for Liver Cancer
If thermal ablation isn’t a good option, we may also be able to destroy tumors by injecting cancer-killing chemicals, such as pure alcohol (ethanol) or acid, directly into them. We reserve this approach for people with three or fewer liver tumors.
NanoKnife for Liver Cancer
We can destroy a primary liver tumor with a minimally invasive NanoKnife® that uses electrical currents (called irreversible electroporation) to punch holes in cancer cell membranes and eliminate them.
Embolization for Liver Cancer
We’re determined to measure how effective these minimally invasive approaches are and what conditions should exist to make them a good option for avoiding the complications that can occur with traditional, open surgery.
Chemotherapy uses chemical substances to destroy cancer cells wherever they are in the body. Depending on your particular situation, we may recommend chemotherapy before surgery to help shrink your liver tumor. This is called adjuvant therapy.
Chemotherapy can also help in lowering the risk that the cancer will come back. This is called neoadjuvant therapy.
For cholangiocarcinoma, we usually prescribe a combination of the chemotherapy agents gemcitabine and cisplatin. Our team also has experience in using other targeted agents, which we may offer to you as part of a clinical trial.
Chemotherapy with Hepatic Arterial Infusion
With this technique, we deliver a high dose of chemotherapy drugs to your hepatic artery (the main source of blood and nutrients for liver tumors) through a small pump that we implant under your skin in the lower abdomen. We can inject more chemotherapy as you may need it through this pump on an outpatient basis.
we can use hepatic arterial infusion (HAI) therapy strategically to shrink your tumors before your surgery or afterward to help prevent them from coming back.
Although it’s a bit different than primary liver cancer, we’ve seen that HAI chemotherapy combined with chemotherapy given in the usual way can dramatically increase how long people live with colon cancer that has spread to the liver, for example. And more recent evidence suggests that HAI chemotherapy alone can lengthen survival in people with primary liver cancer.
A benefit of HAI is that the drugs are delivered to just a part of the body (regionally) rather than system-wide, so it’s less toxic and causes fewer side effects.
Radiation Therapy for Liver Cancer
Radiation therapy can shrink or kill tumor cells. We may recommend this approach if you have a primary liver tumor that can’t be removed with surgery. It can be used alone or in combination with chemotherapy or other treatments.
Both image-guided radiation therapy and respiratory gating have the potential to reduce damage to normal tissue during your treatment.
Image-Guided Radiation Therapy
Image-guided radiation therapy uses real-time imaging with a CT scan or x-rays during radiation therapy to help ensure an ideal setup and lack of motion during treatment. This allows your treatment team to deliver radiation with incredible accuracy.
Respiratory Gating
Because tumors in the liver and organs in the abdomen shift as you breathe, it can be challenging to precisely deliver radiation therapy to cancer tissue. With respiratory gating, we deliver radiation only at certain points during your breathing cycle, when the tumors and certain parts of the liver are in a specific position. This approach decreases the radiation dose to the surrounding healthy tissue.
Follow-Up Care
We believe in staying with you through the whole process and beyond, even after your treatments have ended. Liver cancer usually affects several organs in the body and can be difficult to control. Once we complete the treatment part of your care together, we’ll want to follow your condition and help manage any symptoms or discomforts that might come up.
Through coordinated care from our team of specialists from many areas, we aim to help you have a high quality of life for years to come, much longer than has been possible in years past. Although everyone’s situation is different, regular follow-up care after your first course of treatment will likely include imaging, liver function evaluations, and blood tests.
Be sure to let members of your cancer care team know about any pain, changes, or problems that you experience. Also mention symptoms — such as skin itching, nausea, fever, and jaundice — which may be caused by blockage of the bile ducts. If this happens and the tumor is too widespread to be removed, surgery may help prevent the blockages and reduce your symptoms.
Living Beyond Liver Cancer
we know that even after you’ve finished your cancer treatments, you may still need our help. We’re committed to supporting you in every way we can — physically, emotionally, spiritually, and otherwise — for as long as you need us.
We’ve built a program designed for cancer survivors and their families. Our Survivorship Center has many services for you and your loved ones, including support groups, follow-up programs, educational resources, and more.

